Inspiration and Guidance
Insights
Welcome to Insights!
We are Dr Jo and Dr Dee, PhDs in Counselling Psychotherapy.
As down-to-earth and practical people. We help others to solve problems and find solutions.
Our therapy work is heartfelt and applied to real life.
This blog now newsletter shares our insights over the years - the current version is a re-make of our longstanding blog that began in 2015. As a niche community based project we’ve had over 50,000 visitors to our site during these ten years. That is an impressive accomplishment in Australia.
We hope you enjoy!
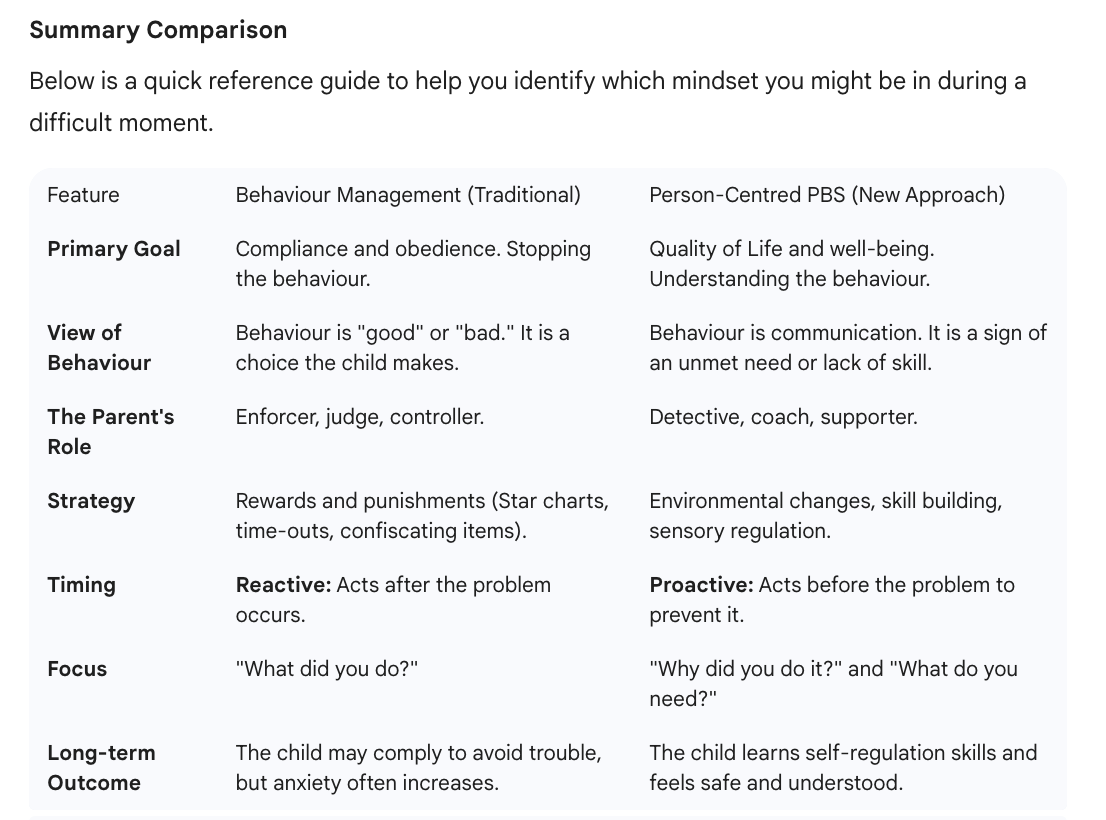
From Controlling the Storm to Understanding the Climate: Moving from Behaviour Management to Positive Behaviour Support
Understanding positive behaviour support is key to parents ability to shift from management to PBS approaches. This article helps to bridge the gap.
Reading Time: Approx. 6 minutes
Introduction: The Parenting tightrope
If you are reading this, you are likely exhausted.
Parenting is a relentless job, and when you are supporting a child with complex needs or challenging behaviours, that exhaustion takes on a different weight.
Most of us were raised in a world of "Behaviour Management." It is the way schools operate, the way our parents raised us, and the way society generally expects us to handle things. If a child does something "good," they get a reward. If they do something "bad," they get a consequence. It sounds logical. It sounds fair.
But if you are reading this, you might have noticed that despite the star charts, the time-outs, the stern voices, and the endless negotiations... the behaviours aren't changing. Or perhaps they stop for a moment, only to explode twice as loud later.
There is a different way. It requires a significant shift in mindset, which can be scary, but it is a shift that moves away from "managing" your child and toward "supporting" them. This is the difference between Behaviour Management and Person-Centred Positive Behaviour Support (PBS).
The Old Way: Behaviour Management
"Behaviour Management" is exactly what it sounds like: it attempts to manage the child. It views the behaviour as the problem that needs to be fixed.
In this model, we often view a meltdown, a hit, or a refusal to listen as "naughty" or "defiant." Our goal becomes compliance. We ask, "How do I make them stop doing that?" and "How do I make them do what I say?"
This approach relies heavily on power and consequences.
The Reward: "If you are quiet in the shop, you get a lolly."
The Punishment: "If you scream, no iPad tonight."
Why it feels like it works (and why it fails)
Behaviour management often works in the short term. If you threaten a consequence, a child might stop the behaviour out of fear or a desire for the reward. This gives us, the parents, a sense of relief. We feel in control.
However, for many neurodivergent children or children with trauma, this approach often backfires.
It ignores the 'Why': It addresses what the child is doing, but not what they are feeling.
It damages connection: It creates a "me vs. you" dynamic. The parent becomes the enforcer rather than the safe harbour.
It assumes skill: It assumes the child could behave if they just wanted to enough. Often, the child wants to do well but lacks the emotional regulation skills to do so.
The New Perspective: Person-Centred Positive Behaviour Support (PBS)
Person-Centred Positive Behaviour Support (PBS) flips the script. Instead of asking "How do I stop this behaviour?", PBS asks "What is this behaviour telling me about my child’s life?"
The core philosophy here is simple but profound: All behaviour is communication.
When your child is screaming, hitting, or shutting down, they are rarely trying to make your life difficult. They are trying to tell you that something is wrong. They might be saying, "I am overwhelmed," "I am in pain," "I am confused," or "I don't feel safe."
PBS doesn't focus on compliance; it focuses on Quality of Life. The theory is that if a child is happy, understood, safe, and engaged in things they love, the challenging behaviour naturally decreases because the need for it disappears.
The Three Pillars of the Shift
To move from Management to Support, we have to change our lens in three specific areas.
1. From "Consequences" to "Adjusting the Environment"
In Behaviour Management, if a child screams in a loud supermarket, we might scold them.
In PBS, we look at the environment. We realize the lights are too bright and the noise is painful for them.
The Fix: We don't punish the scream. We bring noise-cancelling headphones, or we go shopping at a quieter time. We change the world to fit the child, rather than forcing the child to fit the world.
2. From "Stop It" to "Let's Build Skills"
Behaviour Management tries to suppress a behaviour. PBS acknowledges that the behaviour serves a purpose.
If a child hits you to get your attention, Behaviour Management says, "Time out for hitting." The child still needs attention but now doesn't know how to get it.
PBS says, "You need my attention, but hitting hurts. Let's practice tapping me on the shoulder or using a special card when you need me." We teach a replacement behaviour that works better than the hitting.
3. From "Reactive" to "Proactive"
Behaviour Management is usually reactive—we wait for the explosion and then deal with the fallout.
PBS is proactive. We act before the behaviour happens. This is often called the "Green Zone." We want to keep our children in the Green Zone (calm, happy) for as long as possible by meeting their needs early. We feed them before they get "hangry," we provide sensory breaks before they get overwhelmed, and we give warnings before transitions.
A Real-Life Scenario: The Dinner Time Battle
Let’s look at how these two approaches handle a common scenario: A child refuses to sit at the table and throws their food.
The Behaviour Management Approach:
Parent: "Sit down right now or no TV."
Child: Screams and throws peas.
Parent: "That’s it, go to your room. You are being naughty."
Result: The child is hungry and angry; the parent is stressed. The child learns that dinner time is a time of conflict. The root cause (perhaps the chair is uncomfortable, or the social pressure of eating is too high) is never addressed.
The Person-Centred PBS Approach:
Parent (Investigation): Why is this happening? Are their feet dangling? Is the smell of the food overwhelming? Are they too tired to sit upright?
Parent (Action): "I can see you're finding it hard to sit today. Let's try eating this meal at the little table where your feet touch the ground. We can try the big table again tomorrow."
Result: The child eats. The stress remains low. The parent has identified that the child needs more physical stability to eat calmly.
It Is Not Permissive Parenting
A common fear parents have when switching to PBS is: "Am I just letting them get away with it?"
The answer is no. PBS is not about having no boundaries. Safety is still paramount. If a child runs into the road, you stop them. But you don't shame them for it. You stop them to keep them safe, and then later, you look at why they ran and teach them safety skills when they are calm.
PBS is actually more work than behaviour management in the beginning. It requires you to be a detective. It requires patience. It requires you to regulate your own emotions when chaos is happening. But unlike behaviour management, which is a temporary band-aid, PBS builds a future where your child has the skills to cope with the world, and where your relationship is built on trust, not fear.
Moving Forward
If you recognize yourself in the "Behaviour Management" column, please be kind to yourself. You were doing the best you could with the tools you were given. The transition to Positive Behaviour Support is a journey, not a switch you flip overnight.
Start small. The next time a behaviour challenges you, pause. Take a deep breath. Instead of asking, "How do I stop this?", try asking, "What is this telling me?" That single question is the first step toward a happier home.
Working with a PBS Practitioner
The point to this article is, in one sense, that ATS is steeped in personal centred positive behaviour support. We do not practice behaviour management. To work with us means that parents need to make what is sometimes a huge transition.
Even understanding PBS can be challenging - so often our first task in therapy is helping parents to change.
Then, even more radical, our approach to therapy keeps the parents at the centre-circle in PBS methods with the child. We teach the parents how to support their child and also how to parents can ensure that other practitioners or schools come to understand the approach. Parents become empowered to practice PBS and this has the greatest impact for life-long gains.
Positive behaviour support can be for many an investment with a life-long life-changing outcome.
Ten Years of Change Since the NDIS Began in NSW
Amazing 10 years since NDIS launched in NSW and began roll out across Australia - time to reflect and remember.
In July 2016, the National Disability Insurance Scheme (NDIS) started in New South Wales (NSW). It was a big change for people with disabilities, their families, and support workers. Since then, many things have improved and grown. Let’s take a look at some of the important changes in the last ten years.
What is the NDIS?
The NDIS is a government program that helps people with disabilities get the support they need. It gives money for services like therapy, equipment, and support workers. The goal is to help people live more independent lives and be part of their communities.
Seeing through the looking glass.
More People Can Get Help
Since 2016, the NDIS has grown a lot. When it started, only some areas and groups of people could join. Now, almost everyone in NSW who needs help can apply. This means more people with disabilities are getting support than ever before.
Better Services and Support
The NDIS has made many services better. Therapies like physiotherapy, speech therapy, and occupational therapy are easier to access. People can choose the services that fit them best. This choice helps them get the right help for their needs.
Using Technology
Technology has helped the NDIS run more smoothly. Online portals allow people to manage their plans and communicate with workers easily. Especially during times like the COVID-19 pandemic, telehealth services became very important. This means more people can get therapy and advice online, no matter where they live.
Focus on Inclusion
The NDIS encourages inclusion in schools, workplaces, and communities. More programs now support people with disabilities to take part in everyday activities. This helps reduce isolation and creates more opportunities for social connections.
Challenges and Improvements
While there have been many good changes, the NDIS is not perfect. Some people have found the process confusing or slow. The government and providers keep working to fix these problems. They want to make sure everyone gets the help they need without stress.
Looking Ahead
The next ten years will bring more change. The NDIS is working to make plans simpler and support people better. There is a strong focus on listening to participants’ ideas and needs. This will help create a more fair and effective system for everyone.
Conclusion
Since July 2016, the NDIS in NSW has made a big difference. More people can get support, services have improved, and technology helps reach more people. There are still challenges, but the focus on change means the future looks promising for people with disabilities in NSW.
Why People Seek Counselling and Behaviour Support Therapy
Reasons people seek counselling and behaviour therapy are many, and everyone wants a better go. join us to learn more.
Many people look for help through counselling and behaviour support therapy. These services help with different problems in life. They provide support and practical solutions to improve wellbeing and daily living.
Feeling Sad or Anxious
Some people feel very sad or worried for a long time. This might be because of tough events like losing a loved one or dealing with stress at school or work. Counselling helps them talk about their feelings and find ways to feel better.
For example, a teenager might feel anxious about exams. Talking to a counsellor can reduce their stress and teach them ways to manage anxiety.
Struggling with Disability
People with disabilities often face challenges doing everyday tasks. They may find it hard to communicate, learn, or move around easily. Behaviour support therapy helps them find new ways to complete these tasks and live more independently.
For instance, a child with autism might act out when they feel overwhelmed. Behaviour support can teach the child and their family strategies to handle these situations calmly.
Going for a walk is a simple pleasure shared among friends.
Managing Anger or Frustration
Sometimes, people get angry or frustrated and do things they regret. Counselling can help them understand why they feel that way and learn better ways to respond.
An example is an adult who gets angry quickly at work. Therapy can help them recognise triggers and practise calming techniques.
Improving Relationships
Many people seek help to improve their relationships with family, friends, or carers. Counselling offers a safe space to talk about conflicts and learn healthy ways to communicate.
For example, parents of a child with behavioural challenges might need support to understand their child’s needs and how to respond positively.
Coping with Change
Life changes, like moving house, changing jobs, or facing illness, can be hard to handle. Counselling helps people adjust to these changes and build coping skills.
A young adult moving out from home for the first time may feel overwhelmed. Therapy can support them to manage new responsibilities and emotions.
Behaviour Support Plans for Everyday Challenges
People with disabilities sometimes display behaviours that make daily life harder. Behaviour support therapists develop personalised plans to help manage these behaviours safely and respectfully.
For example, a person with intellectual disability might struggle with routine changes. A behaviour support plan can prepare them for transitions and reduce confusion or distress.
Counselling and behaviour support therapy are important tools that help people live happier, more independent lives. They offer practical solutions tailored to each person’s needs and challenges.
Dr Dwayne and Dr Jo are behavioural specialists and counselling therapists. Check out their staff pages here. Give them a ring or send a message in the form on Home Page.
Working together on a project - simple pleasures and more rare and precious than you imagine.
The Jurisprudential Basis for Kinship-Centred Disability Support: Aligning NDIS Funding with UNDRIP and International Human Rights Precedents
A pivotal paper on the inequalities of NDIS policy for Aboriginal Australians - and how to move forward.
Uluru also known as Ayers Rock
Dr Jorandi (Jo) Kisiku Sa’quawei Paq’tism Joseph Randolph Bowers PhD
Executive Summary
The intersection of disability support and Indigenous rights in Australia represents a critical frontier in the pursuit of substantive equality and self-determination. Central to this discourse is the tension between the administrative protocols of the National Disability Insurance Scheme (NDIS)—specifically its restrictive stance on funding family members—and the collective rights of Aboriginal and Torres Strait Islander peoples as articulated in the United Nations Declaration on the Rights of Indigenous Peoples (UNDRIP).
The current NDIS framework is built upon a Western social and medical model of disability that prioritizes individual autonomy and market-based service delivery.1
However, for First Nations Australians, disability is often understood through a cultural lens where the individual’s well-being is inseparable from their connection to family, community, and Country.3
The National Disability Insurance Agency (NDIA) generally prohibits the payment of family members to provide supports, citing a perceived conflict of interest and an expectation that families will provide "informal support" as a matter of course.5
This report argues that this general rule constitutes a form of structural discrimination that fails to account for the unique kinship structures and historical traumas of Indigenous Australians. By drawing on UNDRIP, the National Agreement on Closing the Gap, and international precedents from New Zealand and Canada, a compelling case emerges for a broad and culturally informed exception to the conflict-of-interest rule. This exception is not merely a matter of administrative flexibility but a requirement for compliance with international human rights standards and domestic legal obligations.
The International Human Rights Imperative
UNDRIP and Collective Self-Determination
The United Nations Declaration on the Rights of Indigenous Peoples (UNDRIP), adopted by the UN General Assembly in 2007 and endorsed by Australia in 2009, serves as the authoritative international framework for the protection of Indigenous rights.7
It establishes minimum standards for the survival, dignity, and well-being of Indigenous peoples globally, emphasizing both individual and collective rights.8
For Indigenous Australians with disability, UNDRIP provides a robust legal and moral foundation for demanding that disability supports reflect their cultural identity and social structures.
Articles 3 and 4: The Right to Self-Determination and Autonomy
At the heart of UNDRIP is the right to self-determination. Article 3 states that Indigenous peoples have the right to freely determine their political status and pursue their economic, social, and cultural development.7
In the context of the NDIS, self-determination remains hollow if participants are denied the right to choose the most culturally appropriate and safe person to provide their care.10 When the NDIA imposes an external provider on an Indigenous family, it effectively overrides the participant's right to determine the nature of their social and cultural development.
Article 4 extends this by affirming the right to autonomy or self-government in matters relating to internal and local affairs, as well as the "ways and means for financing their autonomous functions".7
This principle suggests that Indigenous communities should have a degree of control over how NDIS funds are allocated within their kinship networks. Financing an "autonomous function" can be interpreted as funding the existing community-led support systems that have sustained Indigenous people for millennia. The refusal to fund these systems while funding external, often non-Indigenous commercial entities, is a direct contradiction of the right to autonomy in financial and local affairs.3
Article 5: Maintenance of Social and Cultural Institutions
Article 5 upholds the right of Indigenous peoples to maintain and strengthen their "distinct political, legal, economic, social and cultural institutions".7
For Aboriginal and Torres Strait Islander peoples, the extended family or kinship system is the primary social and legal institution. It is the mechanism through which lore is passed, care is managed, and social cohesion is maintained.1
The NDIS’s "informal support" policy—which expects these institutions to operate without financial recognition—undermines their economic viability. By categorizing kinship care as a "conflict of interest" to be avoided, the NDIA treats an essential Indigenous institution as a problem to be mitigated rather than a right to be protected.2
Article 24: The Right to Health and Traditional Practices
Article 24 of UNDRIP specifically addresses the right to health, stating that Indigenous peoples have the right to their traditional medicines and to maintain their "health practices".7
It also affirms that Indigenous individuals have an equal right to the "highest attainable standard of physical and mental health".7
For many First Nations people, the act of a family member providing care is a traditional health practice rooted in cultural concepts of reciprocity and communal responsibility.2
Cultural safety is an essential component of the "highest attainable standard" of health; without it, Indigenous participants frequently experience "double discrimination" and may withdraw from the scheme entirely to avoid traumatizing interactions with culturally incompetent external providers.1
Article 22: Special Needs of Persons with Disabilities
UNDRIP Article 22 explicitly demands that "particular attention shall be paid to the rights and special needs of indigenous elders, women, youth, children and persons with disabilities".7
This creates a positive obligation on the state to tailor its disability schemes to the specific needs of Indigenous people. A one-size-fits-all approach that ignores the primacy of kinship care fails this obligation by not providing the "full protection and guarantees" promised under the declaration.7
The Australian Context
The NDIS and the Conflict-of-Interest Doctrine
The National Disability Insurance Scheme Act 2013 was designed to promote the "independence and social and economic participation" of people with disability.15
However, the operationalization of these goals through the "choice and control" framework often results in a rigid adherence to Western market norms that do not align with Indigenous realities.
The General Rule and the "Informal Support" Expectation
The NDIA’s Operational Guidelines regarding "Sustaining Informal Supports" state that the agency will generally only fund family members to provide supports in "exceptional circumstances".5
The underlying logic is two-fold: first, that paying a family member may be "detrimental to family relationships," and second, that families have a natural obligation to provide unpaid support.6
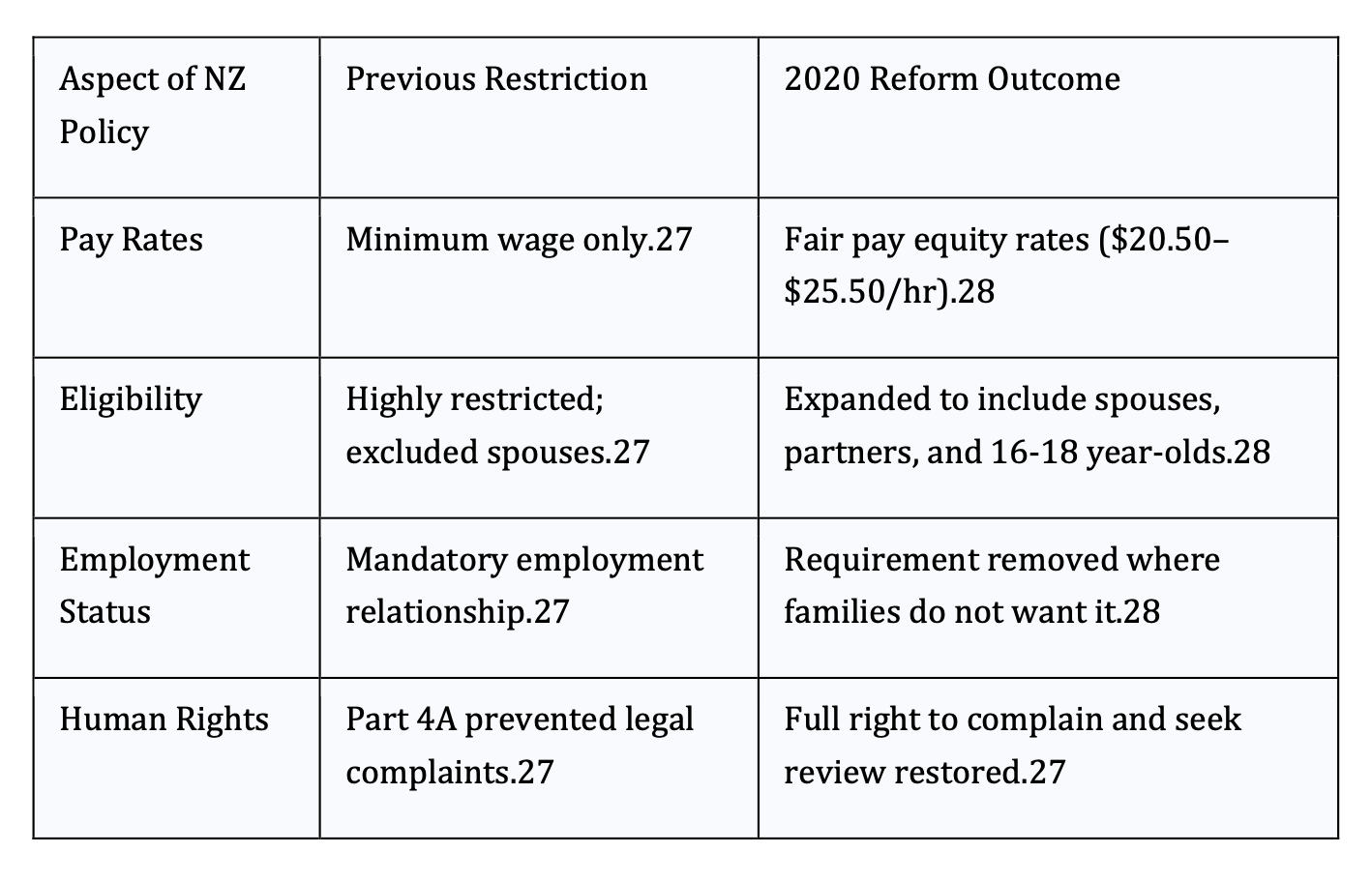
It is argued that these gross and inappropriate assumptions are inherently colonial in bias and institutionally imbalanced in practice. The following table shows the structural and practical impact of these prejudicial policies on Indigenous Australian families.
Defining "Exceptional Circumstances"
The NDIA currently recognizes three broad categories of exceptional circumstances where family members may be paid:
1 Risk of Harm or Neglect: When the participant would be unsafe with an external provider.5
2 Religious or Cultural Reasons: When cultural norms dictate that only certain people can provide intimate or close care.20
3 Strong Personal Views: When the participant’s dignity or privacy is at stake.5
While these exceptions exist, they are often applied so narrowly that they become inaccessible to many First Nations participants. The burden of proof placed on a family to demonstrate that they are the only suitable provider is often insurmountable, particularly when the NDIA adopts a "deficit-focused model" that ignores the strengths of Indigenous kinship systems.17
Thin Markets and the Failure of Choice
The market-based model of the NDIS assumes that there is a pool of providers from which a participant can choose.
In many remote and regional areas, this market is non-existent.1
The Disability Royal Commission found that the lack of available, accessible, and culturally appropriate services for First Nations people is a "national crisis".24
In these "thin markets," the choice is not between a family member and a culturally safe external provider; it is between a family member and no support at all.3 Refusing to fund a family member in a region where no other provider exists is a failure to provide "reasonable and necessary" supports as required by Section 34 of the NDIS Act.19
International Precedents for Family-Based Funding Models
Comparative analysis of other Commonwealth nations reveals that Australia's restrictive approach is out of step with global trends toward Indigenous self-determination in social services.
The New Zealand Model: Whānau Ora and Funded Family Care
New Zealand’s Whānau Ora framework is a world-leading example of a culturally grounded, holistic approach to disability and health. It puts the whānau (extended family) at the centre of decision-making, acknowledging that individual well-being is dependent on collective health.25
In 2020, the New Zealand government significantly reformed its "Funded Family Care" policy to address human rights concerns. Previously, New Zealand had legislation (Part 4A of the NZ Public Health and Disability Act) that limited the rights of families to challenge funding decisions.27 The repeal of this discriminatory law allowed for a more compassionate and rights-based approach. The table below highlights these reforms.
The New Zealand experience demonstrates that paying family members does not degrade the quality of care; rather, it "restores dignity" and recognizes the "important work family carers do".27 For Māori and Pacific families, who make greater use of these schemes, this policy is an essential tool for health equity.28
The Canadian Precedent: Jordan's Principle and Substantive Equality
In Canada, the legal framework for Indigenous disability care is driven by the principle of "substantive equality." This is most clearly seen in "Jordan's Principle," a child-first legal rule ensuring First Nations children can access all government-funded services without delays caused by jurisdictional disputes.29
Following a series of rulings by the Canadian Human Rights Tribunal, the federal government was found to have discriminated against First Nations children by narrowly defining essential services and underfunding Indigenous-led agencies.31 This led to a historic $23.34 billion settlement for families who were denied or delayed in receiving services.29
Furthermore, Canada's An Act respecting First Nations, Inuit and Métis children, youth and families (2020) affirms the "inherent right" of Indigenous peoples to exercise jurisdiction over their own child and family services.33
This provides a direct precedent for Indigenous Australians to argue that the NDIA must respect Indigenous-led designs of service delivery, including those that prioritize kinship care over external commercial providers.
National Policy Drivers
Closing the Gap and the Royal Commission
The Australian policy landscape is shifting toward a greater recognition of Indigenous sovereignty and the need for structural reform in disability services.
The National Agreement on Closing the Gap (2020)
The National Agreement on Closing the Gap is a pledge by all Australian governments to "do things differently" by working in genuine partnership with Aboriginal and Torres Strait Islander communities.35
The agreement is built around four "Priority Reforms" that directly challenge the current NDIS operating model.
Priority Reform 1: Shared Decision-Making: Governments must give Indigenous people a say in all decisions that affect them.35
This includes the design of individual NDIS plans and the choice of providers.
Priority Reform 2: Building the Community-Controlled Sector: Funding should be prioritized for organizations designed and controlled by Aboriginal people.35
A kinship-based funding model is the ultimate form of a "community-controlled" service.
Priority Reform 3: Transforming Government Organisations: Governments must address unconscious bias and systemic racism in their processes.35
The categorical dismissal of kinship care as a "conflict of interest" can be analysed as a systemic bias that devalues Indigenous social structures.
Findings of the Disability Royal Commission
The Royal Commission into Violence, Abuse, Neglect and Exploitation of People with Disability (2023) highlighted that Indigenous people with disability are "culturally safe when people understand, respect and celebrate their First Nations identity".4
The Commission recommended that governments fund First Nations Community Controlled Organisations to provide "flexible supports and services".4
Crucially, the Commission acknowledged that "cultural safety, family, community, and connectedness are central to service delivery and engagement".40
This creates a powerful mandate for the NDIS to move away from the mainstream as well as "medical model" toward a "cultural model of inclusion".3
Legal Mechanisms for Advocacy
Human Rights Acts and the ART
Advocates in Australia have several domestic legal levers to challenge restrictive NDIA decisions regarding family funding.
The Queensland Human Rights Act 2019
The Human Rights Act 2019 (Qld) is a significant piece of legislation for Indigenous Australians. It protects fundamental human rights, including the "cultural rights of Aboriginal peoples and Torres Strait Islander peoples".41
Section 28 of the Act specifically protects the right of Indigenous people to:
· Maintain and strengthen their distinct political, legal, economic, social, and cultural institutions.41
· Conserve and maintain their heritage and distinctive spiritual and cultural practices.42
Under Section 58 of the Act, "public entities" (which include registered NDIS providers and government departments) must act and make decisions in a way that is compatible with these human rights.43
An NDIS decision that refuses to fund a kinship-based support model could be seen as an unlawful limitation on the right of an Indigenous family to maintain their cultural institutions.42 While the NDIS is a federal scheme, the High Court and superior courts have increasingly recognized that state-based human rights obligations can influence the exercise of administrative discretion by federal delegates.41
The Administrative Review Tribunal (ART) and Merits Review
Participants who are dissatisfied with an NDIA internal review can appeal to the Administrative Review Tribunal (formerly the AAT). The Tribunal conducts a "merits review," meaning it steps into the shoes of the NDIA to make the "preferable decision".46
Advocates appearing before the Tribunal can argue that:
Cultural Necessity is an "Exceptional Circumstance": Drawing on the Operational Guidelines to prove that external care is inappropriate for the specific participant’s cultural needs.5
Market Failure and Reasonableness: Arguing that in the absence of other providers, funding a family member is the only "reasonable and necessary" way to achieve the goals in the participant's plan.4
Consistency with NDIS Objects: Arguing that Section 4 of the NDIS Act requires the role of families and carers to be "acknowledged and respected," which should extend to financial support in circumstances of economic hardship and service gaps.15
The Economic and Social Impact of Reform
The refusal to fund kinship care is not just a human rights issue; it is a failed economic policy that perpetuates intergenerational poverty.
Quantifying the Service Gap
Indigenous NDIS participants are 28% less likely to receive care than non-Indigenous participants.24
The "utilization gap" represents a significant failure in the NDIS’s promise of equity: it is the difference between the funding the government legally allocates to a participant and the amount that is actually spent on their care. Currently, First Nations participants utilize their funding at a rate of 72%, significantly lower than non-Indigenous participants .
This disparity is most acute in remote regions where "thin markets"—the total absence of external service providers—prevent participants from spending their budgets . We can calculate this systemic failure as a "Lost Benefit" ($B_{lost}$) to the community using the following model:
$$B_{lost} = F \times (1 - U_{util})$$
Where $F$ is the total funding allocated and $U_{util}$ is the utilization rate.
When the utilization rate ($U_{util}$) drops in remote areas, the "Lost Benefit" to the community is maximized.
By refusing to pay family members for care, the NDIA ensures this money remains unspent in government coffers rather than being used to support the participant. Reforming this rule would allow these funds to be "reclaimed" by the community. Instead of unspent potential, the funding would become a local salary, creating an economic multiplier that supports Indigenous employment and acts as a preventative safeguard against the types of family crises that lead to state-driven child removal .
Breaking the Cycle of Child Removal
A critical "third-order" insight is the relationship between NDIS funding and child protection.
In the Tennant Creek case, the withdrawal of NDIS funding for a boy with cerebral palsy led directly to his removal by the state.48
This highlights how rigid administrative rules can inadvertently contribute to "Closing the Gap" failures, particularly Target 12 (reducing the rate of children in out-of-home care).38
Funding kinship care is therefore a "safeguard" that promotes and protects an individual's right to live with their family.6
Actionable Recommendations for NDIS Advocacy
Based on the research and international precedents, advocacy for an exception to the conflict-of-interest rule should be framed around the following pillars:
Asserting UNDRIP Compliance: Argue that the NDIS Act must be interpreted consistently with UNDRIP Articles 3, 5, and 24. Any decision that ignores the primacy of kinship care is a breach of the right to self-determination and the maintenance of cultural institutions.7
Documenting Market Failure: In areas with no culturally safe providers, advocates must demand that the NDIA fulfill its "reasonable and necessary" obligation by funding the only available support: the family.1
Leveraging the First Nations Strategy: Use the NDIA’s own First Nations Strategy 2025-2030 to hold the agency accountable to its commitments of "community-centred" and "culturally safe" support.49
Challenging the "Informal Support" Myth: Dispute the assumption that Indigenous families have an "unlimited" capacity for unpaid labour. Highlight that in contexts of systemic poverty, "informal support" is a luxury that families cannot afford without sacrificing their own health and economic security.1
A Mandate for Structural Change
The data around the rights of Indigenous Australians reveals a profound disconnect between the aspirational language of the NDIS and the bureaucratic reality of its implementation.
The "conflict of interest" rule, while well-intentioned in a commercial context, acts as a barrier to cultural safety and self-determination when applied to Indigenous kinship networks.
The United Nations Declaration on the Rights of Indigenous Peoples provides the necessary framework to challenge this status quo. Combined with the successes of the Whānau Ora model in New Zealand and the "substantive equality" victories in Canada, the path forward is clear:
The NDIS must move beyond viewing family members as a "risk" and instead recognize them as the most effective, culturally safe, and sustainable providers of disability support.
The "cultural reasons" exception must be broadened from a rare, grudgingly granted concession to a standard operating procedure for First Nations participants.
This shift is not only supported by international law and national agreements like Closing the Gap but is essential for the NDIS to fulfill its promise of an inclusive and equitable Australia.
By funding the kinship structures that have always cared for Indigenous people, the NDIS can transition from a colonial institution of "structural neglect" into a genuine partner in Indigenous well-being and self-determination.
While we live in hope – hope is not enough for our current clients who are stuck in the colonial wheels of a mechanistic system that disempowers their voice, denies their cultural wisdom, and prevents them from exercising fundamental human rights to choice and control informed by their cultural and undisputed historical sovereignty.
For families dealing with crisis now, today, the NDIS presents an administrative system that even within escalated complex cases under senior planners continues to deny funding even when clinical needs are argued by medical and specialist expert analysis and under reasonable and necessary criteria.
This paper reflects on the discomforting nature of the NDIA as a broken institution that practices inequitable delivery of funding and demonstrates numerous biases and prejudicial policies and practices. These issues very much require attention and reform. But more so, current NDIS participants who are Indigenous Australians deserve so much better.
Action to address Indigenous NDIS participant’s needs must happen now – not in future years or under some future reform agenda.
Works cited
1. Improving Disability Services for Aboriginal People in the Northern Territory | AMSANT, accessed December 18, 2025, https://www.amsant.org.au/wp-content/uploads/2025/03/Improving-Disability-Services-for-Aboriginal-People-in-the-Northern-Territory.pdf
2. Full article: Indigenous experiences and underutilisation of disability support services in Australia: a qualitative meta-synthesis - Taylor & Francis Online, accessed December 18, 2025, https://www.tandfonline.com/doi/full/10.1080/09638288.2023.2194681
3. The NDIS Workforce and First Nations People, accessed December 18, 2025, https://www.ndisreview.gov.au/sites/default/files/2023-11/FPDN_Workforce_Paper.pdf
4. Final Report - Volume 9, First Nations people with disability, accessed December 18, 2025, https://disability.royalcommission.gov.au/publications/final-report-volume-9-first-nations-people-disability
5. Has anyone had family approved as paid support due to culture? : r/NDIS - Reddit, accessed December 18, 2025, https://www.reddit.com/r/NDIS/comments/1jmhf3h/has_anyone_had_family_approved_as_paid_support/
6. Informal Supports - Peer Connect, accessed December 18, 2025, https://www.peerconnect.org.au/oldsite/index.php/download_file/544/534/
7. United Nations Declaration on the Rights of Indigenous Peoples and In Plain Sight - Gov.bc.ca, accessed December 18, 2025, https://engage.gov.bc.ca/app/uploads/sites/613/2021/03/UNDRIP-and-IPS-FINAL.pdf
8. UN Declaration on the Rights of Indigenous Peoples | OHCHR, accessed December 18, 2025, https://www.ohchr.org/en/indigenous-peoples/un-declaration-rights-indigenous-peoples
9. United Nations Declaration on the Rights of Indigenous Peoples, accessed December 18, 2025, https://www.un.org/development/desa/Indigenouspeoples/wp-content/uploads/sites/19/2018/11/UNDRIP_E_web.pdf
10. TRANSFORMING DISABILITY ACCESS for Indigenous Australians, accessed December 18, 2025, https://www.iuih.org.au/wp-content/uploads/2024/05/IUIH-Submission-Disability-Royal-Commission.pdf
11. United Nations Declaration on the Rights of Indigenous Peoples, accessed December 18, 2025, https://www.un.org/esa/socdev/unpfii/documents/DRIPS_en.pdf
12. Support coordinators and conflict of interest | NDIS, accessed December 18, 2025, https://www.ndis.gov.au/providers/working-provider/support-coordinators/support-coordinators-and-conflict-interest
13. Conflicts of interest in the NDIS provider market, accessed December 18, 2025, https://www.ndis.gov.au/providers/provider-compliance/conflicts-interest-ndis-provider-market
14. The United Nations Declaration on the Rights of Indigenous Peoples - ohchr, accessed December 18, 2025, https://www.ohchr.org/Documents/Issues/IPeoples/UNDRIPManualForNHRIs.pdf
15. Empowering the Unpaid Carer in the NDIS Framework - Special Voices, accessed December 18, 2025, https://www.specialvoices.com.au/empowering-the-unpaid-carer-in-the-ndis-framework/
16. Including Specific Types of Supports in Plans - NDIS, accessed December 18, 2025, https://www.ndis.gov.au/media/8008/download?attachment
17. Can I Be My Child's NDIS Support Worker? - 24seven Plan Management, accessed December 18, 2025, https://24sevenplanmanagement.com.au/am-i-allowed-to-be-my-childs-support-worker/
18. What are conflicts of interest? (DOCX 54.9KB) - NDIS, accessed December 18, 2025, https://www.ndis.gov.au/media/7392/download?attachment
19. OG - Reasonable and Necessary Supports | PDF | Caregiver | Disability - Scribd, accessed December 18, 2025, https://www.scribd.com/document/910151450/OG-Reasonable-and-Necessary-Supports
20. Your burning questions answered - My Plan Manager, accessed December 18, 2025, https://myplanmanager.com.au/burning-ndis-questions-answered/
21. Reasonable and Necessary Supports | NDIS, accessed December 18, 2025, https://www.ndis.gov.au/media/7772/download?attachment
22. Download Delivering Parent Pathways Guidelines – Part B - Department of Employment and Workplace Relations, accessed December 18, 2025, https://www.dewr.gov.au/download/16588/delivering-parent-pathways-guidelines-part-b-operational-guidance/41183/delivering-parent-pathways-guidelines-part-b-operational-guidance/docx
23. We contest the NDIA's justification for NDIS independent assessments - People with Disability Australia, accessed December 18, 2025, https://pwd.org.au/wp-content/uploads/2021/04/SUPP-SUB-08042021_JSC-Critique-of-NDIA-Independent-Assessment-Submission.._.pdf
24. The lack of NDIS services for First Nations people with disability 'a national crisis', accessed December 18, 2025, https://disability.royalcommission.gov.au/news-and-media/media-releases/lack-ndis-services-first-nations-people-disability-national-crisis
25. Whānau Ora | RANZCP, accessed December 18, 2025, https://www.ranzcp.org/clinical-guidelines-publications/clinical-guidelines-publications-library/whanau-ora
26. The Whānau Ora Outcomes Framework - Te Puni Kōkiri - Ministry of Māori Development, accessed December 18, 2025, https://www.tpk.govt.nz/docs/tpk-wo-outcomesframework-aug2016.pdf
27. Government restores fairness for family carers | Beehive.govt.nz, accessed December 18, 2025, https://www.beehive.govt.nz/release/government-restores-fairness-family-carers
28. Government to deliver family carers $2000 pay rise, expand scheme to spouses this year, accessed December 18, 2025, https://www.beehive.govt.nz/release/government-deliver-family-carers-2000-pay-rise-expand-scheme-spouses-year
29. FAQ | First Nations Child and Family Services and Jordan's Principle Settlement, accessed December 18, 2025, https://fnchildclaims.ca/resources-support/faq/
30. Without denial, delay, or disruption: - Canadian Child Welfare Research Portal, accessed December 18, 2025, https://cwrp.ca/sites/default/files/publications/jpreport_final_en.pdf
31. Reformed Approach to Child and Family Services, accessed December 18, 2025, https://fncaringsociety.com/sites/default/files/2024-03/38504%20Reformed%20Approach%20to%20CFS%20v7f.pdf
32. Timeline: Jordan's Principle and First Nations child and family services, accessed December 18, 2025, https://www.sac-isc.gc.ca/eng/1500661556435/1533316366163
33. Celebrating Five Years of Indigenous-led Child and Family Services Law - Canada.ca, accessed December 18, 2025, https://www.canada.ca/en/indigenous-services-canada/news/2025/01/celebrating-five-years-of-indigenous-led-child-and-family-services-law.html
34. Annual Report to Parliament 2024 - Indigenous Services Canada, accessed December 18, 2025, https://www.sac-isc.gc.ca/eng/1728913460798/1728913482672
35. National Agreement on Closing the Gap | Communities and Justice - NSW Government, accessed December 18, 2025, https://dcj.nsw.gov.au/content/dcj/dcj-website/dcj/community-inclusion/improving-aboriginal-outcomes/national-agreement.html
36. Closing the Gap | NIAA - National Indigenous Australians Agency, accessed December 18, 2025, https://www.niaa.gov.au/our-work/closing-gap
37. The National Agreement on Closing the Gap - Coalition of Peaks, accessed December 18, 2025, https://www.coalitionofpeaks.org.au/national-agreement-on-closing-the-gap
38. Closing the Gap - Australian Government Department of Social Services, accessed December 18, 2025, https://www.dss.gov.au/closing-gap
39. Closing the Gap - Parliament of Australia, accessed December 18, 2025, https://www.aph.gov.au/About_Parliament/Parliamentary_departments/Parliamentary_Library/Research/Briefing_Book/47th_Parliament/ClosingTheGap
40. Summary and Overview: - Royal Commission into Violence, Abuse, Neglect, and Exploitation of people with Disability Final Report - Mental Health Coordinating Council, accessed December 18, 2025, https://mhcc.org.au/wp-content/uploads/2023/11/MHCC_Summary_-Overview_-Disability-Royal-Commission-4F-7.11.2023.pdf
41. Human Rights Law in Queensland, accessed December 18, 2025, https://queenslandlawhandbook.org.au/wp-content/uploads/2022/06/64.-human-rights-law-in-queensland-december-2020.pdf
42. Human Rights Act 2019 - Queensland Legislation, accessed December 18, 2025, https://www.legislation.qld.gov.au/view/whole/html/current/act-2019-005
43. Human rights | Your rights, crime and the law - Queensland Government, accessed December 18, 2025, https://www.qld.gov.au/law/your-rights/human-rights
44. Human Rights of People with Disability - Queensland Law Handbook, accessed December 18, 2025, https://queenslandlawhandbook.org.au/the-queensland-law-handbook/health-and-wellbeing/disability-and-the-law/human-rights-of-people-with-a-disability/
45. Strengthening Queensland's human rights act, accessed December 18, 2025, https://brq.org.au/strengthening-queenslands-human-rights-act/
46. National Disability Insurance Scheme | Administrative Review Tribunal, accessed December 18, 2025, https://www.art.gov.au/applying-review/national-disability-insurance-scheme
47. Chapter 10 – Parliament of Australia, accessed December 18, 2025, https://www.aph.gov.au/Parliamentary_Business/Committees/Joint/National_Disability_Insurance_Scheme/NDISPlanning/Final_Report/section?id=committees%2Freportjnt%2F024487%2F73192
48. Tennant Creek boy with cerebral palsy placed in care after NDIA pulls funding | National disability insurance scheme | The Guardian, accessed December 18, 2025, https://www.theguardian.com/australia-news/2018/jul/11/tennant-creek-boy-with-cerebral-palsy-placed-in-care-after-ndia-pulls-funding
49. First Nations Strategy | NDIS, accessed December 18, 2025, https://www.ndis.gov.au/strategies/first-nations-strategy
Disclaimer
The content provided in this article is for general informational purposes only and does not constitute legal, clinical, or specialist behaviour support advice. It should not be relied upon as such.
All information is provided in good faith, however, we make no representation or warranty of any kind, express or implied, regarding the accuracy, adequacy, validity, reliability, or completeness of any information. The information pertaining to NDIS and related issues must be individually determined by each person’s circumstances and their specialist therapist teams, and is a very complex evolving context and support needs and methods are subject to change.
This article is not a substitute for professional advice from your qualified GP or specialist for from your NDIS Behaviour Support Practitioner. You should always consult with an appropriate professional to address your specific circumstances. Under no circumstance shall Ability Therapy Specialists Pty Ltd have any liability to you for any loss or damage incurred as a result of the use of this information. Reliance on any information provided in this post is solely at your own risk. This article, website, and your participation are governed under the Client Booklet - Privacy Policy: Disclaimer, Terms, Conditions as a necessary provision under Australian service quality standards.
The Evolving Landscape of Autism Support (2020–2025): Neurological Mechanisms, Applied Interventions, and the Paradigm Shift in Level 2 Care
An in-depth discussion of the most recent research findings for Autism Level 2 Support up to and including 2025.
Coloured circles on white background with the letters A U T I S M on small square blocks.
Editor’s Note
This post comes from our study of Autism - by way of wanting to review the literature up to the end of 2025. When I was researching, my interests were to review findings on state of the art support and therapy for behavioural support. Because many of our cases tend to be ASD Level 2, Requiring Substantial Support, this was my choice of focus for this particular moment.
This is an in-depth post. It may take about 30-40 minutes to read once, and you will find yourself needing to read it at least two times. While that is a big time investment, you will not find this level of information in many places. Our work in these lengthy posts is to provide a curated summary of high quality and value.
Like our work with clients, we tend to be comprehensive when necessary and when useful to the person’s support needs and funding reviews. I hope you find this information useful and helpful. To our Australian readers, I apologise for the spelling and terminology - the international nature of the research as well as the dominant voice appears to have an American tone. I gave a thot to changing/editing the paper once we had the first draft completed, and simply do not have the time before Christmas this year.
We appreciate this paper - because the science confirms much of our clinical experience and moves our understanding further due to the significant insights from recent scientific findings. We suspect that with the dawn of AI post 2025, the next 2-5 years will see significant advances in our understanding Autism from medical, psychotherapeutic, and disability support perspectives.
A word of caution - this paper is NOT clinical advice at all. People are advised to seek your behaviour specialist, occupational therapist, or medical doctor for treatment specific questions. This paper is in fact an exploration of the literature to gain insights about new advances in high level clinical perspectives. In fact, many of the insights here are more relevant to American contexts for example, the paper highlights certain treatment shifts in the USA.
Our primary audience is Australian - and this paper’s weakness is that it does not translate and discuss implications to the Australian context. That said, sharing this paper rather than holding it back for 3-4 months to write more seemed the most practical. It is up to therapists, doctors, and specialists to take this information and explore implications and treatment options in local contexts.
For parents and people with Autism, copy the URL of this page and share this with your GP or therapist. Ask them to read the information, and to provide you with practical advice. Rely on your GP and your specialist therapist input - do not rely on anything you read here. The pace of change and what is most relevant or current is shifting very quickly - get your advice from your GP and the therapist specialists they recommend.
- Dr Jorandi (Joseph Randolph) Bowers PhD
1. Introduction: The State of Autism Research and Practice in 2025
The half-decade between 2020 and 2025 represents a seminal epoch in the history of autism research, characterized by a fundamental decoupling of "pathology" from "identity" and a simultaneous explosion in mechanistic biological understanding. As the prevalence of Autism Spectrum Disorder (ASD) in the United States has risen to approximately 1 in 31 children as of 2025—a figure that demands robust public health and educational responses—the scientific community has moved beyond merely describing symptoms to elucidating the neural circuitries that drive them.1
For individuals classified as requiring "Level 2" support (Substantial Support Needs), this era has been transformative. Historically, this demographic—often characterized by marked deficits in verbal and nonverbal social communication skills, social impairments apparent even with supports in place, and limited initiation of social interactions—occupied a precarious middle ground. They were often too "complex" for light-touch interventions yet possessed potential for autonomy that was frequently stifled by the heavy-handed custodial models used for Level 3 populations.3 The research of 2025 has corrected this imbalance, offering targeted, dignity-affirming, and biologically grounded strategies specifically for those with substantial support needs.
The convergence of molecular neuroscience and social science has yielded a dualistic progression. On one front, the "Medical Model" has achieved unprecedented granularity, identifying specific thalamocortical gating failures and synaptic pruning deficits that explain sensory overwhelm with physiological precision.4 On the other, the "Social Model" and the neurodiversity movement have reshaped clinical ethics, forcing a departure from compliance-based therapies toward those that prioritize regulation, autonomy, and mental health.6
This paper synthesizes the exhaustive body of literature from 2020 through late 2025, providing a comprehensive analysis of the neurological underpinnings of emotional regulation, the efficacy of Naturalistic Developmental Behavioral Interventions (NDBI), the critical role of the Low Arousal Approach, and the emerging technological landscape supporting executive function. It serves as a roadmap for clinicians, researchers, and families navigating the complex terrain of substantial support needs in 2025.
1.1 Prevalence, Demographics, and the Identification Gap
The epidemiology of autism has shifted dramatically. The Centers for Disease Control and Prevention (CDC) reported in April 2025 that the prevalence of ASD had reached 3.2% (1 in 31) of 8-year-old children, a sharp increase from 1 in 36 just two years prior.1 This rise is not merely a statistical artifact of better counting; it reflects a broadening of diagnostic criteria and improved identification in historically underserved communities.
However, disparities persist. While identification has improved, the "diagnosis age" remains stagnant at an average of 4 years, despite the American Academy of Pediatrics recommending screening at 18 and 24 months.7 This delay is critical for Level 2 support, as early intervention windows for establishing communication systems are often missed. Furthermore, the 2025 data indicates that while 1 in 3 children with autism also has an intellectual disability, the specific needs of the "Level 2" cohort—who may have average IQ but severe adaptive functioning deficits—are often obscured in aggregate data.2
1.2 The Autism Data Science Initiative (ADSI)
Recognizing the complexity of these demographic shifts, the National Institutes of Health (NIH) launched the Autism Data Science Initiative (ADSI) in late 2024. This $100 million endeavor utilizes advanced machine learning and "exposome-wide" analyses to disentangle the gene-environment interactions contributing to the rising prevalence.1 Unlike previous genomic studies that sought a "smoking gun," ADSI focuses on heterogeneity, attempting to map specific biological subtypes (biotypes) to specific support needs. This initiative represents a move toward "precision medicine" in autism, where a child’s specific neural connectivity profile could eventually dictate whether they receive sensory integration therapy, pharmaceutical support, or intensive communication coaching.
2. Neurological Frontiers: Brain Function, Connectivity, and Emotional Regulation
The interval from 2020 to 2025 has been pivotal in moving beyond descriptive neuroanatomy to mechanistic understandings of autistic brain function. The "black box" of the autistic brain—particularly regarding why sensory inputs often lead to catastrophic emotional dysregulation—has been illuminated by breakthrough findings in thalamic gating and synaptic architecture. These findings are not merely academic; they provide the physiological rationale for the "Low Arousal" and "Sensory Safety" therapeutic approaches discussed later in this report.
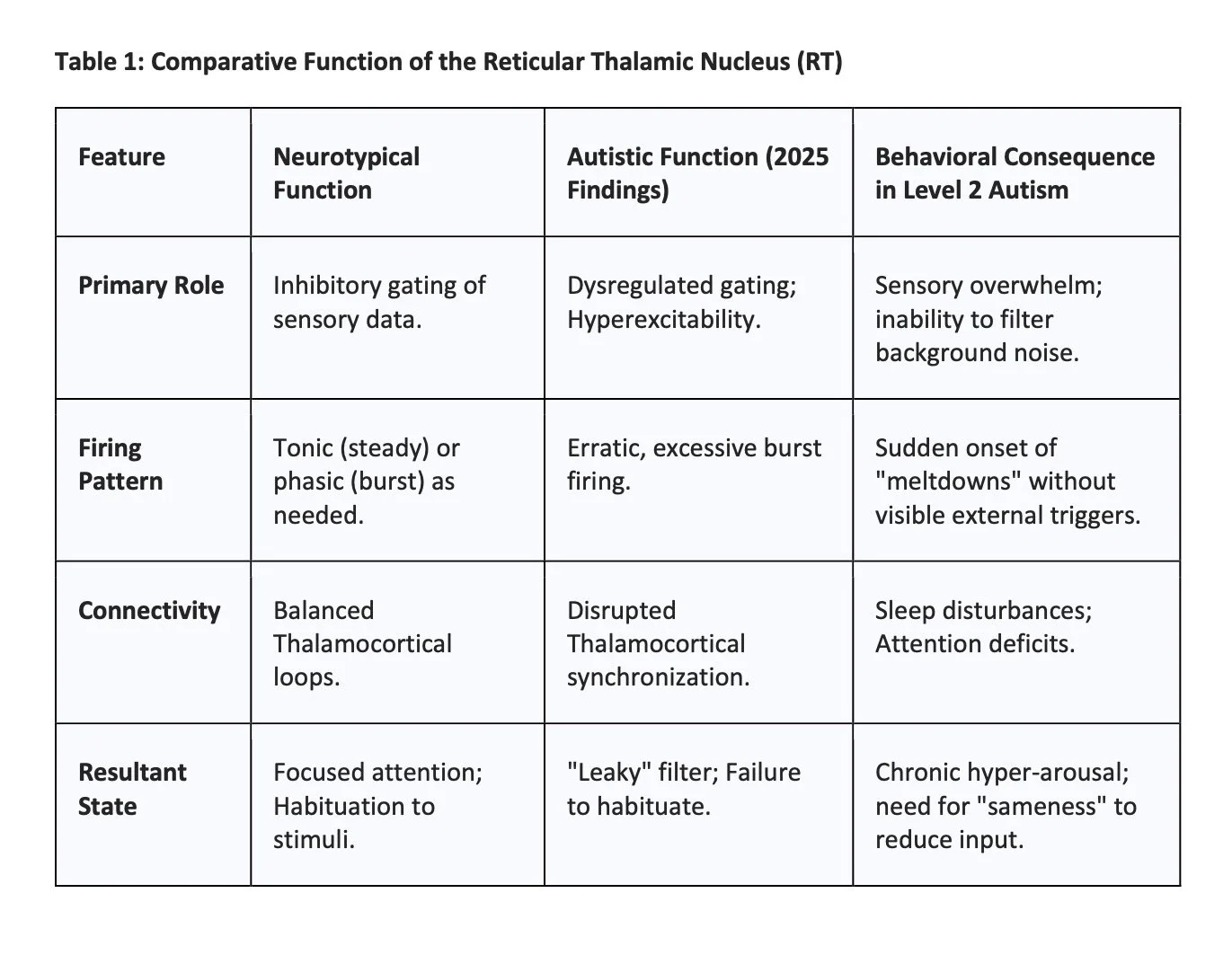
2.1 The Reticular Thalamic Nucleus: The Gatekeeper of Consciousness
One of the most consequential findings of 2025 is the identification of the Reticular Thalamic Nucleus (RT) as a primary driver of sensory and behavioral anomalies in autism. Research conducted at Stanford Medicine and published in Science Advances (August 2025) has elucidated that hyperactivity in the RT—a shell-like structure acting as a "gatekeeper" for sensory information—can drive behaviors traditionally associated with autism, such as social withdrawal and repetitive movements.4
2.1.1 The "Leaky Thalamus" Hypothesis and Sensory Gating
The thalamus serves as the central relay station for sensory information (visual, auditory, tactile) traveling from the periphery to the cortex. It is the brain's mixing board. The RT, composed largely of inhibitory GABAergic neurons, regulates this flow. In neurotypical functioning, the RT inhibits or "gates" irrelevant background noise (e.g., the hum of an air conditioner, the feeling of a tag on a shirt), allowing the cortex to focus on salient information.
The 2025 findings, utilizing the Cntnap2 knockout mouse model (a robust genetic model for autism), revealed that the RT in autistic brains exhibits hyperexcitability and burst firing.12 This hyperexcitability paradoxically disrupts the gating mechanism. Instead of smoothly filtering stimuli, the RT functions erratically, potentially allowing an overwhelming flood of sensory data to reach the cortex—a phenomenon termed the "leaky thalamus" hypothesis.14
For an individual with Level 2 autism, this means the brain is literally besieged by unfiltered sensory data. The behavioral output—covering ears, humming, or retreating—is not "non-compliance" but a physiological necessity to manage cortical saturation.
2.1.2 Causal Links and Therapeutic Implications
The causal link established in the Stanford study is robust. Researchers utilized chemogenetics (DREADDs) to manipulate the RT. When they suppressed the hyperactivity of the RT using a specific drug (Z944, a T-type calcium channel blocker), they observed a reversal of autism-like behaviors. The mice showed improved social interactions and reduced repetitive behaviors.4 Conversely, stimulating the RT in neurotypical mice induced autism-like behaviors.
This finding overlaps significantly with epilepsy research. Epilepsy is present in approximately 30% of autistic individuals compared to 1% of the general population.9 The shared mechanism of thalamic hyperexcitability suggests that drugs targeting these specific calcium channels could serve dual purposes: managing seizures and reducing the painful intensity of sensory processing disorders in autistic populations.
2.2 Synaptic Density and the Hyper-Connectivity Theory
Parallel to the functional findings in the thalamus, structural imaging studies in 2024 and 2025 have solidified the theory of altered synaptic pruning. A landmark study utilizing Positron Emission Tomography (PET) scans with the radiotracer 11C-UCB-J allowed researchers to visualize synaptic density in living brains for the first time, moving beyond post-mortem analysis.5
2.2.1 The Pruning Deficit
During typical development, the brain produces an excess of synapses in early childhood, which are subsequently "pruned" during adolescence to increase efficiency and signal clarity. The 2025 data indicates that autistic brains retain a significantly higher density of synapses. In some cortical regions, the reduction in synapses during adolescence was found to be only 16% in autistic brains, compared to the typical 50% drop observed in neurotypical controls.15
This finding challenges the older "under-connectivity" theories. The autistic brain is likely hyper-connected at the local level. While this density might theoretically support enhanced memory or attention to detail (strengths often seen in Level 2 autism), it creates a "noisy" neural environment.16
2.2.2 Functional Implications of Hyper-Connectivity
The retention of excess synapses correlates with the "Intense World Theory" of autism. A brain with too many connections may process specific stimuli with excruciating intensity but struggle to integrate information across distant brain regions (long-range under-connectivity).
Monotropism: The hyper-connected local networks may explain "monotropism," the tendency to have a singular, intense focus. The neural hardware is wired to lock onto one stream of information deeply, making "task switching" (which requires disengaging that robust local network) metabolically expensive and emotionally distressing.17
Sensory Amplification: Combined with the RT dysfunction, high synaptic density ensures that once sensory data breaches the thalamic gate, it is amplified by the dense cortical networks, leading to rapid overstimulation.
2.3 Neural Circuits of Emotional Regulation
Emotional dysregulation—rapid shifts in mood, prolonged distress, and difficulty returning to baseline—is a core challenge for individuals with substantial support needs. Research through 2025 has mapped these challenges to specific disconnects between the Prefrontal Cortex (PFC) and the Limbic System.
2.3.1 The Prefrontal-Amygdala Disconnect
Functional MRI (fMRI) studies involving cognitive reappraisal tasks—where participants are asked to "reframe" a negative image to reduce their emotional response—have shown distinct activation patterns in autistic adults.
Neurotypical Response: Regulation involves increased activation of the Dorsolateral Prefrontal Cortex (DLPFC), which sends inhibitory signals to the Amygdala (fear center) and Nucleus Accumbens (reward/emotion center), effectively "cooling down" the reaction.
Autistic Response: The 2025 studies found that while autistic participants understood the task, their brains showed significantly less modulation of the Amygdala and Nucleus Accumbens by the PFC.18
This suggests a mechanistic decoupling: the "top-down" regulatory commands from the PFC do not effectively reach or influence the "bottom-up" emotional centers. This provides a physiological basis for why cognitive strategies (e.g., "Tell yourself it's okay," "Count to ten") are often ineffective for Level 2 autistic individuals during moments of high arousal. The neural pathway required for logic to soothe emotion is functionally impaired.
2.3.2 Structural Variations: Amygdala and Hippocampus
Structural analyses have further nuanced our understanding of the "social brain." While earlier studies offered conflicting data on amygdala size, 2025 consensus points toward developmental trajectories where the amygdala is often enlarged in early childhood (linked to anxiety and over-responsivity) and remains structurally distinct in adulthood.16 Furthermore, the hippocampus, critical for memory, is often enlarged. This may explain the intense, specific memories associated with special interests or, conversely, the deep encoding of traumatic sensory events (e.g., a specific loud fire alarm) that can trigger phobic responses years later.16
2.4 Interoception and the Insular Cortex
A critical area of research that bridges neurology and therapy is Interoception—the sensing of internal bodily states (hunger, heart rate, bladder fullness, pain). The Insular Cortex (Insula) is the primary hub for interoception. Research indicates that autistic individuals often show hypo-activity or aberrant connectivity in the right Anterior Insula (rAI) and its interaction with the Default Mode Network (DMN).20
2.4.1 The Mechanism of Alexithymia
This insular dysfunction provides the neurological mechanism for Alexithymia (difficulty identifying and describing emotions), which affects approximately 50% of the autistic population. If the brain does not accurately process the physiological signals of an emotion (e.g., recognizing a racing heart as "anxiety" or a growling stomach as "hunger"), the individual cannot label the state or engage in regulation until the physical sensation becomes overwhelming.
Implication for Level 2 Support: Behaviors labeled as "sudden aggression" are often the result of unrecognized internal pain or hunger that the individual could not feel until it reached a threshold of agony. The "Interoceptive Discrimination Difficulty" is a primary target for modern therapeutic interventions.21
3. The Paradigm Shift: Neurodiversity-Affirming Practice in 2025
The period from 2020 to 2025 has witnessed a decisive ethical and clinical pivot. The "Medical Model," which views autism as a set of deficits to be cured or normalized, has been largely superseded in research and progressive practice by the "Neurodiversity Paradigm." This shift is particularly critical for Level 2 support, where the intensity of intervention previously led to restrictive or compliance-based practices that are now recognized as harmful.
3.1 From Compliance to Autonomy
Traditional behavioral approaches often prioritized "compliance"—teaching a child to follow directions immediately, maintain "quiet hands," or suppress stimming (self-stimulatory behavior). By 2025, a significant body of literature, including guidelines from professional bodies like the American Occupational Therapy Association (AOTA), has re-evaluated these goals.6
3.1.1 The Trauma of "Quiet Hands" and Masking
Research into Autistic Burnout has identified "masking" (the suppression of autistic traits to fit in) as a primary contributor to mental health crises, depression, and suicidality in autistic adults.24 Interventions that enforce "quiet hands" or forced eye contact are now understood to increase cognitive load and anxiety, thereby reducing the capacity for genuine learning or social connection.
The 2025 Consensus: Stimming is a necessary regulatory mechanism. Suppressing it deprives the individual of a tool to manage the "leaky thalamus" discussed in Section 2.
Clinical Shift: Therapists are now trained to distinguish between harmful behaviors (self-injury) and autistic behaviors (flapping, rocking). The latter are to be respected and protected.17
3.2 The Double Empathy Problem
The Double Empathy Problem, a theory proposed by Dr. Damian Milton, has gained robust empirical support through 2024-2025. It posits that communication breakdowns between autistic and non-autistic people are mutual, not solely the fault of the autistic person.
Research Findings: Studies show that autistic people communicate effectively with other autistic people; the transfer of information is accurate and rapport is high. The "deficit" only appears in mixed neurotype interactions.17
Impact on Therapy: This shifts the burden of intervention. Instead of solely training the autistic individual to mimic neurotypical social skills, interventions now focus on "two-way" understanding. Families, teachers, and peers are trained to interpret autistic communication styles (e.g., infodumping, echolalia, avoidance of eye contact) as valid and meaningful.25
3.3 Neuro-Affirming Goal Setting
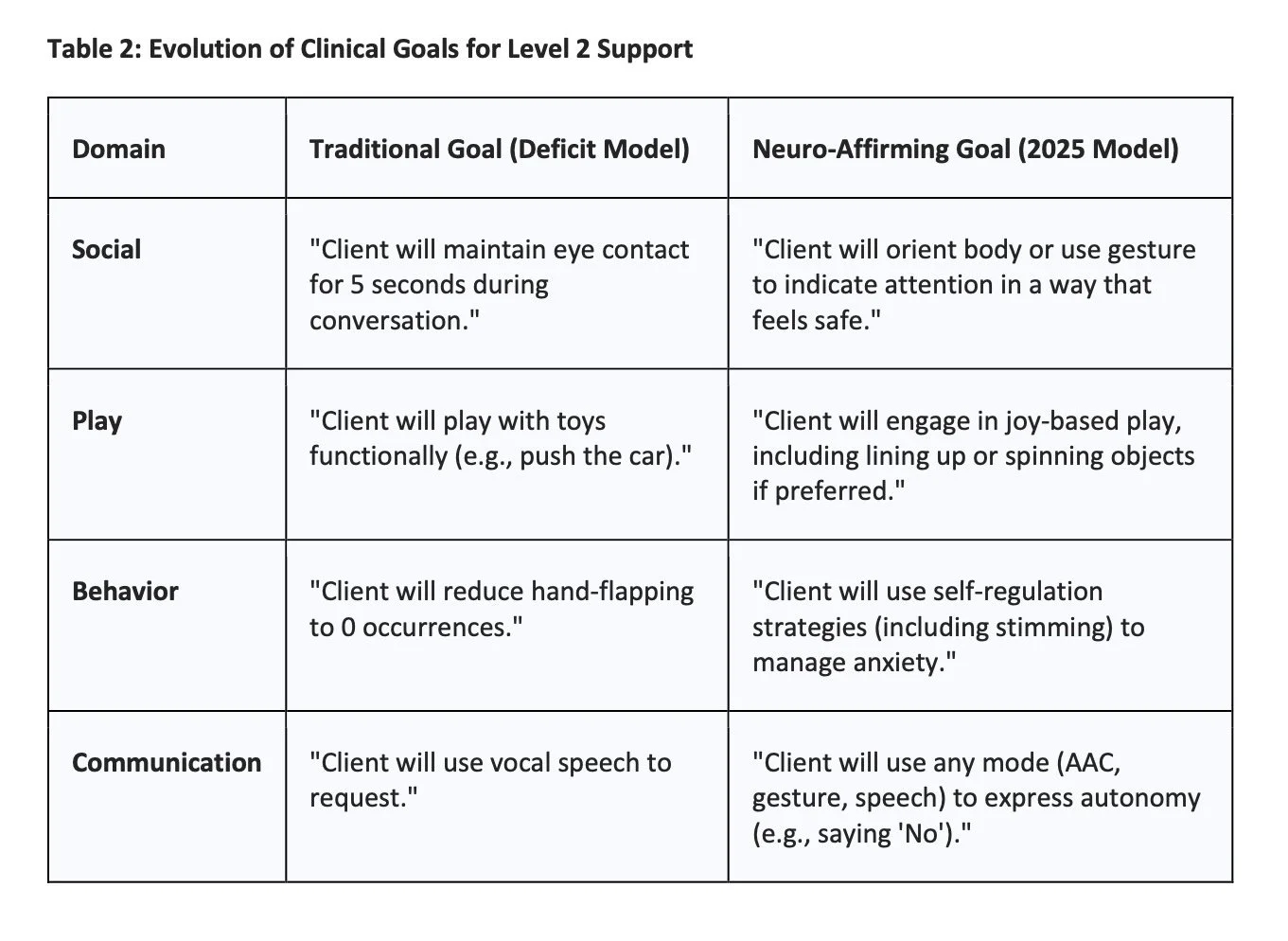
In 2025, clinical goals for substantial support needs have moved away from "normalization" toward "quality of life" and "self-determination."
This shift is documented in updated frameworks for speech-language pathology and occupational therapy, which explicitly warn against goals that induce masking.17
4. Applied Therapeutics for Substantial Support Needs (Level 2)
Individuals with Level 2 autism require "substantial support." The 2020-2025 research literature highlights that effective intervention for this group must be intensive yet naturalistic, robustly supported by technology, and centered on physiological regulation rather than behavioral suppression.
4.1 Naturalistic Developmental Behavioral Interventions (NDBI)
NDBIs represent the evolution of behavioral science, merging the principles of Applied Behavior Analysis (ABA) with developmental science. Unlike Discrete Trial Training (DTT), which occurs in a structured, often artificial setting, NDBIs (such as JASPER, Early Start Denver Model, and Project ImPACT) are implemented in natural environments like play and daily routines.
4.1.1 Efficacy in Group and Telehealth Settings
Recent studies (2024-2025) have validated the scalability of NDBIs, which is crucial given the shortage of providers.
Group-Based NDBI: A study published in Journal of Speech, Language, and Hearing Research (2025) examined group-based NDBI for young autistic children. It demonstrated significant increases in "active engagement" and social relatedness over a 10-month period.28 The study highlighted that while the group average improved, individual trajectories varied based on baseline social pragmatic skills, suggesting that Level 2 children may need "priming" or 1:1 breakout sessions to fully benefit from group work.
Telehealth Efficacy: A mixed-methods pilot study of Project ImPACT delivered via telehealth showed statistically significant decreases in peer interaction challenges.30 This confirms that parents can be effectively coached to deliver high-fidelity NDBI strategies at home, a vital finding for addressing health equity in underserved regions.
4.2 The Low Arousal Approach
For individuals with Level 2 support needs, who may experience frequent dysregulation or "meltdowns" due to the thalamic gating issues described earlier, the Low Arousal Approach has emerged as a gold standard in crisis management.31
4.2.1 Mechanism and Application
The approach is predicated on the understanding that challenging behavior is often a panic response (Fight/Flight) fueled by sensory and emotional overload.
Reducing Demands: In a moment of escalation, the immediate goal is safety, not compliance. The Low Arousal protocol dictates dropping all demands to lower the cognitive load.
Sensory Reduction: Interventions involve lowering lights, reducing verbal input (stopping the "talking at" the person), and increasing physical space to reduce the perception of threat.
Affect Regulation: The caregiver must manage their own emotional state ("Peace of mind is contagious") to prevent emotional contagion, where the caregiver's stress further escalates the autistic individual.32
Unlike restraint or seclusion, which increase physiological arousal and trauma, this approach aims to lower the "temperature" of the interaction. It shifts the focus from "consequences" to "antecedent management"—changing the environment before the crisis occurs.
4.3 Augmentative and Alternative Communication (AAC)
For Level 2 individuals, communication barriers are a primary source of frustration and behavior. The 2025 landscape for AAC emphasizes "Robust AAC" systems and the presumption of competence.
4.3.1 Moving Beyond "Requesting"
Historically, AAC for substantial support needs often focused on "wants and needs" (e.g., asking for a cookie). Current best practices 34 emphasize a Core Vocabulary approach—teaching high-frequency words (go, stop, more, help, different) that allow for a wide range of communicative functions, including commenting, protesting, and asking questions.
4.3.2 Techno-Ableism and Multi-Modal Communication
A critical 2025 discourse involves "techno-ableism"—the assumption that high-tech devices are superior or curative. Research cautions that while speech-generating devices are powerful, they must not replace multi-modal communication.36 Gestures, leading an adult by the hand, vocalizations, and low-tech picture boards are all valid forms of language. The goal is autonomous communication, not just the use of a device.
4.4 Interoception-Based Interventions
Given the insular hypoconnectivity and alexithymia common in Level 2 autism, teaching interoception has become a therapeutic priority. The work of Kelly Mahler and others has been adapted specifically for non-speaking clients.37
4.4.1 The Curriculum for Non-Speakers
Standard interoception curricula often rely on verbal dialogue ("How does your stomach feel?"). Adaptations for 2025 involve:
Modeling: The therapist narrates their own bodily sensations ("I am yawning; my energy feels low").
Tactile Exploration: Using "Body Experiments" (e.g., holding an ice cube vs. a warm towel) to help the individual connect sensation to vocabulary without requiring verbal output.39
Co-Regulation: Using the therapist's regulated state to help the client feel safe enough to notice internal signals.40
4.5 Peer-Mediated Instruction and Intervention (PMI)
PMI involves training neurotypical peers to support autistic students. While highly effective for social inclusion, 2025 reviews note a gap in research for students with substantial support needs.41 However, when adapted—for instance, training peers to use the autistic student's AAC device or to engage in the autistic student's preferred "special interest" play—PMI promotes genuine inclusion and breaks down social isolation.42
5. Daily Life Assistance, Executive Function, and Technology
For individuals with Level 2 autism, the "executive function" gap—planning, organizing, initiating tasks, and working memory—is often a greater barrier to independence than social deficits. The 2020-2025 period has seen a surge in "Assistive Tech" that acts as a prosthetic for executive function.
5.1 AI-Driven Executive Function Support
Artificial Intelligence has moved from novelty to utility in autism support. By 2025, apps like Tiimo and Thruday utilize AI to create dynamic, visual schedules that adapt to the user's needs.44
Predictive Scheduling: Newer algorithms can analyze behavioral data (if integrated with wearables) to predict "triggers." If a user typically becomes dysregulated after 20 minutes of a specific task, the AI can suggest a break before the meltdown occurs.46
Visualizing Time: Time blindness is a common feature of autism. Apps that use visual timers (e.g., a disappearing red disk) provide concrete representations of abstract concepts, reducing anxiety during transitions.47
5.2 Video Modeling for Daily Living Skills (DLS)
Acquiring daily living skills (hygiene, cooking, cleaning) is a primary goal for Level 2 support. Video Modeling has proven exceptionally effective for this population.
Mechanism: It bypasses the social-processing demand of face-to-face instruction. The individual watches a video of the task (from a first-person perspective) and imitates it. This aligns with the "visual learning" strength of many autistic people.
2025 Efficacy Data: Case studies and meta-analyses confirm that video modeling is effective for complex chains of behaviors (e.g., washing dishes, doing laundry) and that skills are maintained over time without the need for constant supervision.49
Implementation: Using tablets to display the video step-by-step at the point of performance (e.g., an iPad mounted in the bathroom playing a "brushing teeth" clip) allows for real-time prompting.
5.3 Safety Skills and Elopement
Elopement (wandering) remains a critical safety concern for Level 2 families. Interventions in 2025 focus on Behavioral Skills Training (BST) and environmental modification.
Water Safety: Given the high risk of drowning, specialized swim instruction that includes clothes-on swimming and safety commands is essential. Programs now focus on "survival swimming" rather than stroke technique.52
Tech Solutions: Passive measures like GPS trackers and door alarms are standard, but active safety involves teaching "stop" commands using high-reinforcement protocols (e.g., practicing stopping at a curb for a high-value reward).53
5.4 Transition Support Strategies
Transitions are a flashpoint for dysregulation due to Monotropism (the intense, single-track focus of the autistic mind). Evidence-based strategies for substantial support needs include:
Priming: Warning the individual about what is coming next well in advance to allow for cognitive shifting.
Visual Countdowns: Using a visual countdown (5-4-3-2-1 cards) rather than just a verbal one, which may be missed if auditory processing is overwhelmed.
Transitional Objects: Allowing a preferred item (e.g., a toy car) to travel from activity A to activity B to maintain a sense of continuity and safety.47
6. The Lifespan Perspective: Adulthood and Systemic Support
The "Services Cliff"—the drastic reduction in support after high school—remains a critical issue in 2025. With 1 in 31 children now diagnosed, the wave of autistic adults entering the system is unprecedented.1
6.1 The State of Adult Services
Employment: While 8 out of 10 eligible autistic adults enroll in job training, only half secure employment. This discrepancy highlights a systemic failure in "transition" planning and workplace accommodation. The focus is often on training the individual, rather than modifying the workplace to be sensory-friendly.57
Housing: 1 in 4 families with an autistic child faces housing insecurity, exacerbated by the lack of specialized, affordable adult housing options that provide Level 2 support (e.g., semi-independent living with drop-in support).57
Day Programs: For Level 2 adults, day programs are shifting from "custodial care" to "community integration." Programs like Avondale House and university-based initiatives (e.g., IMPACT at the University of Cincinnati) focus on vocational skills, communication, and recreation rather than mere supervision.58
6.2 Social Isolation and Mental Health
Loneliness is a significant health risk for autistic adults, comparable to smoking in its physical effects. Research in 2025 clarifies that autistic adults desire connection but often lack the "neuro-affirming" spaces to find it.60
Affinity Groups: Groups based on shared interests (Special Interests) are more successful than general "social skills" groups. When autistic adults gather around a shared passion (e.g., anime, coding, trains), social barriers often dissolve.
Adult Support Groups: Organizations like AANE and The Autism Project offer online and in-person groups that validate autistic identity rather than trying to "cure" it. These "closed" groups allow adults to discuss burnout, sensory issues, and navigation of the neurotypical world with peers who understand.62
7. Pharmacological, Genetic, and Medical Updates (2025)
While behavioral and educational interventions are primary, 2025 has seen notable medical updates relevant to Level 2 support, particularly concerning co-occurring metabolic and genetic conditions.
7.1 Leucovorin and Cerebral Folate Deficiency (CFD)
In September 2025, the FDA initiated approval for Leucovorin calcium for patients with Cerebral Folate Deficiency (CFD).64
Mechanism: CFD is a condition where folate (vitamin B9) cannot cross the blood-brain barrier due to the presence of autoantibodies. This deficiency leads to developmental delays, seizures, and autistic symptoms. Leucovorin is a reduced folate that bypasses this blocked transport mechanism.
Relevance: CFD is highly comorbid with autism (and often undiagnosed). Treating the folate deficiency can lead to significant improvements in speech and social interaction for the subset of autistic individuals with this metabolic profile.
7.2 Prenatal Acetaminophen (Tylenol) Warnings
The FDA has issued updated warnings regarding the use of acetaminophen during pregnancy, citing a "considerable body of evidence" suggesting a correlation (though not definitively causal) with increased risks of autism and ADHD.66 This remains a contentious area, but the shift in guidance represents a precautionary approach in prenatal care.
7.3 Genetic Architecture and Personalized Medicine
Research has identified 230 new genes linked to ASD as of 2024.9 The Autism Data Science Initiative (ADSI) is currently using machine learning to parse how these genes interact with environmental factors.1 This supports the move toward "personalized medicine," where interventions might eventually be tailored to an individual's specific genetic and neural profile (e.g., treating those with the Cntnap2 variance with RT-targeting therapies, while others might benefit more from oxytocin-pathway interventions).
8. Conclusion: A New Era of Informed Support
The research of 2020-2025 has coalesced into a clear, evidence-based narrative for Level 2 support: Intervention must be biologically informed but humanistically delivered.
We have moved beyond the "black box" era. We now understand the biological reality of sensory overwhelm (the Reticular Thalamic Nucleus), the structural reality of hyper-connectivity (Synaptic Density), and the social reality of the Double Empathy Problem.
8.1 Key Takeaways for Support Providers
Respect the Neurology: Use Low Arousal strategies not just because they are "nice," but because the Level 2 brain is physiologically wired for intensity and lacks the gating mechanisms to filter noise.
Prioritize Interoception: Teach the individual to feel their body (heart rate, tension) before expecting them to regulate their behavior. Emotional regulation is impossible without interoceptive awareness.
Leverage Technology: Use AI scheduling and video modeling to bypass executive function deficits, acting as a digital prosthetic for the frontal lobe.
Affirm Identity: Ensure that social support validates the autistic experience. Stop fighting the symptoms (stimming, monotropism) and start supporting the person (autonomy, safety, connection).
By aligning support strategies with the biological reality of the autistic brain—respecting its intense connectivity and unique sensory gating—we can build lives of quality, connection, and dignity for individuals with substantial support needs. The future of autism support is not about "fixing" the individual, but about optimizing the environment and the understanding of those around them.
Works cited
Autism Announcement Fact Sheet | HHS.gov, accessed December 13, 2025, https://www.hhs.gov/press-room/autism-announcement-fact-sheet.html
CDC Community Report on Autism 2025, accessed December 13, 2025, https://www.cdc.gov/autism/media/pdfs/2025/04/ADDM-Community-Report-SY2022.pdf
High-Level Support in Autism - Apex ABA Therapy, accessed December 13, 2025, https://www.apexaba.com/blog/high-level-support-in-autism
Repurposed epilepsy drugs show potential for new autism therapies - Drug Target Review, accessed December 13, 2025, https://www.drugtargetreview.com/news/184268/repurposed-epilepsy-drugs-show-potential-for-new-autism-therapies/
A Key Brain Difference Linked to Autism Is Found for the First Time in Living People, accessed December 13, 2025, https://medicine.yale.edu/news-article/a-key-brain-difference-linked-to-autism-is-found-for-the-first-time-in-living-people/
Affirming Neurodiversity within Applied Behavior Analysis - PMC - PubMed Central - NIH, accessed December 13, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11219658/
Facts About Autism: Comprehensive Overview for 2025 - Abacus Therapies, accessed December 13, 2025, https://abacustherapies.com/facts-about-autism-comprehensive-overview-for-2024/
Science Updates About Autism Spectrum Disorder (ASD), accessed December 13, 2025, https://www.nimh.nih.gov/news/science-updates/autism-spectrum-disorder-asd
Promising Autism Research Breakthroughs in 2025: New Hope for Understanding and Treatment, accessed December 13, 2025, https://linksaba.com/promising-autism-research-breakthroughs/
Stanford study shows autism-like behaviors can be switched off in mice - PsyPost, accessed December 13, 2025, https://www.psypost.org/stanford-study-shows-autism-like-behaviors-can-be-switched-off-in-mice/
Hyperactivity in reticular thalamic nucleus drives autism-like behaviors in mice, accessed December 13, 2025, https://www.news-medical.net/news/20250820/Hyperactivity-in-reticular-thalamic-nucleus-drives-autism-like-behaviors-in-mice.aspx
Reticular Thalamic Hyperexcitability Drives Autism Spectrum Disorder Behaviors in the Cntnap2 Model of Autism | bioRxiv, accessed December 13, 2025, https://www.biorxiv.org/content/10.1101/2025.03.21.644680v1.full-text
Reticular thalamic hyperexcitability drives autism spectrum disorder behaviors in the Cntnap2 model of autism - PMC - PubMed Central, accessed December 13, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC12366697/
Thalamic functional connectivity and sensorimotor processing in neurodevelopmental disorders - PMC - PubMed Central, accessed December 13, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10755010/
Children with Autism Have Extra Synapses in Brain, accessed December 13, 2025, https://www.cuimc.columbia.edu/news/children-autism-have-extra-synapses-brain
Autistic Brain vs Normal Brain: Decoding Neurodiversity - Yellow Bus ABA, accessed December 13, 2025, https://www.yellowbusaba.com/post/autistic-brain-vs-normal-brain
Neurodiversity-Affirming Therapy: Positions, Therapy Goals, and Best Practices, accessed December 13, 2025, https://therapistndc.org/neurodiversity-affirming-therapy/
Neural Mechanisms of Emotion Regulation in Autism Spectrum Disorder - PubMed Central, accessed December 13, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4515208/
Neural Mechanisms of Emotion Regulation in Autism Spectrum Disorder, accessed December 13, 2025, https://cdr.lib.unc.edu/concern/articles/cf95jk09n
Mapping brain functional and structural abnormities in autism spectrum disorder: moving toward precision treatment - Oxford Academic, accessed December 13, 2025, https://academic.oup.com/psyrad/article/2/3/78/6815557
Ask a Lurie Center Researcher: Autism and Interoception: Understanding the Body's Hidden Signals, accessed December 13, 2025, https://www.massgeneral.org/assets/mgh/pdf/children/lurie-center-lurienow-autism-and-interoception.pdf
Occupational Therapy Practice Guidelines for Autistic People Across the Lifespan, accessed December 13, 2025, https://research.aota.org/ajot/article/78/3/7803397010/25188/Occupational-Therapy-Practice-Guidelines-for
Moving Toward Neurodiversity-Affirming Occupational Therapy for Autistic People: Key Questions and Next Steps - WMU's ScholarWorks, accessed December 13, 2025, https://scholarworks.wmich.edu/cgi/viewcontent.cgi?article=2244&context=ojot
2025 Neurodiversity Affirming Practice Speakers - STAR Institute, accessed December 13, 2025, https://sensoryhealth.org/basic/2025-neurodiversity-affirming-practice-speakers
Neurodiversity Affirming Therapy Practices: Complete Guide - ABA & Autism Therapy Services, accessed December 13, 2025, https://kctherapy.com/neurodiversity-affirming-therapy-practices/
Autism and communication - National Autistic Society, accessed December 13, 2025, https://www.autism.org.uk/advice-and-guidance/topics/about-autism/autism-and-communication
Neurodivergent-Affirming SLT | AutisticSLT, accessed December 13, 2025, https://www.autisticslt.com/nd-affirmingslt
Effects of an Inclusive Group-Based Naturalistic Developmental Behavioral Intervention on Active Engagement in Young Autistic Children: A Preliminary Study - PubMed, accessed December 13, 2025, https://pubmed.ncbi.nlm.nih.gov/39879478/
Effects of an Inclusive Group-Based Naturalistic Developmental Behavioral Intervention on Active Engagement in Young Autistic Children: A Preliminary Study - Johns Hopkins University, accessed December 13, 2025, https://pure.johnshopkins.edu/en/publications/effects-of-an-inclusive-group-based-naturalistic-developmental-be/
Telehealth Pilot Study of the Effects of a Naturalistic Developmental Behavioral Intervention on Child Social Communication Outcomes in a Community Mental Health System - MDPI, accessed December 13, 2025, https://www.mdpi.com/2076-328X/15/9/1171
The Low Arousal Approach: A Practitioner's Guide - BCU Open Access Repository - Birmingham City University, accessed December 13, 2025, https://www.open-access.bcu.ac.uk/6544/1/the-low-arousal-approach.pdf
Low Arousal and Effective Crisis Management in a World of Noise - Studio 3, accessed December 13, 2025, https://www.studio3.org/post/low-arousal-and-effective-crisis-management-in-a-world-of-noise
What is the Low Arousal Approach and How Can It Benefit My Family?, accessed December 13, 2025, https://autismawarenesscentre.com/what-is-the-low-arousal-approach-and-how-can-it-benefit-my-family/
AAC in Autism, accessed December 13, 2025, https://www.advancedautism.com/post/aac-in-autism
Communication in Autistic Adults: An Action-Focused Review - PMC - PubMed Central, accessed December 13, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC12271282/
Full article: Dismantling societal barriers that limit people who need or use AAC: lived experiences, key research findings, and future directions - Taylor & Francis Online, accessed December 13, 2025, https://www.tandfonline.com/doi/full/10.1080/07434618.2025.2508490
On-Demand Course: Interoception and the Non-Speaking Client - Kelly Mahler, accessed December 13, 2025, https://www.kelly-mahler.com/product/on-demand-course-interoception-and-the-non-speaking-client/
Interoception and Non-Speaking/Verbal Autistic Clients | Kelly Mahler, accessed December 13, 2025, https://www.kelly-mahler.com/interoception-non-speaking-autistic/
Interoception: Body Awareness Exercises - Autism Connection of Pennsylvania, accessed December 13, 2025, https://autismofpa.org/interoception-body-awareness-exercises-for-autistic-children/
Interoception and the Non-Speaking Client | Kelly Mahler Blog, accessed December 13, 2025, https://www.kelly-mahler.com/resources/blog/interoception-and-the-non-speaking-client/
A systematic review of peer-mediated interventions for children with autism spectrum disorder - NIH, accessed December 13, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC5087797/
Peer-Mediated Instruction in Autism, accessed December 13, 2025, https://www.advancedautism.com/post/peer-mediated-instruction-in-autism
Peer-Mediated Instruction And Intervention In Autism, accessed December 13, 2025, https://www.ambitionsaba.com/resources/peer-mediated-instruction-and-intervention-in-autism
Neuroinclusive AI Planning | Smarter, Adaptive Support for ADHD & Autism - Tiimo App, accessed December 13, 2025, https://www.tiimoapp.com/resource-hub/ai-planner
Thruday | Visual Planner & To-Do App for ADHD & Autism, accessed December 13, 2025, https://thruday.com/
Latest Advancements in Autism Therapy: 2025 Trends to Watch - AB Spectrum, accessed December 13, 2025, https://www.abspectrum.org/advancements-in-autism-therapy-2025/
Transition Time: Helping Individuals on the Autism Spectrum Move Successfully from One Activity to Another, accessed December 13, 2025, https://iidc.indiana.edu/irca/articles/transition-time-helping-individuals-on-the-autism-spectrum-move-successfully-from-one-activity-to-another.html
Using Technology to Support Executive Functioning Skills in Adults with Autism, accessed December 13, 2025, https://gershautismacademy.com/blog/using-technology-to-support-executive-functioning-skills-in-adults-with-autism/
EJ1373145 - Video Modeling and Daily Living Skills Training in Students with ASD, Journal of Educational Sciences, 2022 - ERIC, accessed December 13, 2025, https://eric.ed.gov/?id=EJ1373145
Examining the Effects of Video Modeling and Prompts to Teach Activities of Daily Living Skills - NIH, accessed December 13, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC5118254/
Teaching Daily Living Skills to Children with Autism Through Instructional Video Modeling, accessed December 13, 2025, https://www.researchgate.net/publication/247784937_Teaching_Daily_Living_Skills_to_Children_with_Autism_Through_Instructional_Video_Modeling
ABA strategies for teaching safety skills - Ambitions ABA Therapy, accessed December 13, 2025, https://www.ambitionsaba.com/resources/aba-strategies-for-teaching-safety-skills
Strategies For Enhancing Safety For Autistic Children - Autism Learning Partners, accessed December 13, 2025, https://autismlearningpartners.com/nurturing-safety/
Teaching Safety Skills to Children: A Discussion of Critical Features and Practice Recommendations - PMC - NIH, accessed December 13, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC9582057/
Children, Autism, and Change: Tips to Make Transition Easier | Brown University Health, accessed December 13, 2025, https://www.brownhealth.org/be-well/children-autism-and-change-tips-make-transition-easier
Improving Transition to Adulthood for Students with Autism: A Randomized Controlled Trial of STEPS - PubMed Central, accessed December 13, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC8513749/
2025 Autism by the Numbers Annual Report now live, accessed December 13, 2025, https://www.autismspeaks.org/science-news/2025-autism-numbers-annual-report-now-live
Adult Day Program - Avondale House, accessed December 13, 2025, https://www.avondalehouse.org/services-adult-day-program
ADULT DAY ARRAY GUIDE 2025 - Hamilton County Developmental Disabilities Services, accessed December 13, 2025, https://www.hamiltonddsohio.gov/wp-content/uploads/2025/04/2025-ADA-Provider-Guide-2.pdf
Friendship, Loneliness and Belonging in Autistic People - Reframing Autism, accessed December 13, 2025, https://reframingautism.org.au/friendship-loneliness-and-belonging-in-autistic-people/
Experiences of friendship among autistic adults: a scoping review - PMC - PubMed Central, accessed December 13, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC12034726/
Autistic Adult - AANE, accessed December 13, 2025, https://aane.org/autistic-adult/
Finding your community | Autism Speaks, accessed December 13, 2025, https://www.autismspeaks.org/finding-your-community
FDA Takes Action to Make a Treatment Available for Autism Symptoms, accessed December 13, 2025, https://www.fda.gov/news-events/press-announcements/fda-takes-action-make-treatment-available-autism-symptoms
President Trump, Secretary Kennedy Announce Bold Actions to Tackle Autism Epidemic, accessed December 13, 2025, https://www.hhs.gov/press-room/hhs-trump-kennedy-autism-initiatives-leucovorin-tylenol-research-2025.html
FDA Responds to Evidence of Possible Association Between Autism and Acetaminophen Use During Pregnancy, accessed December 13, 2025, https://www.fda.gov/news-events/press-announcements/fda-responds-evidence-possible-association-between-autism-and-acetaminophen-use-during-pregnancy
Mount Sinai Study Supports Evidence That Prenatal Acetaminophen Use May Be Linked to Increased Risk of Autism and ADHD, accessed December 13, 2025, https://www.mountsinai.org/about/newsroom/2025/mount-sinai-study-supports-evidence-that-prenatal-acetaminophen-use-may-be-linked-to-increased-risk-of-autism-and-adhd
Disclaimer
The content provided in this article is for general informational purposes only and does not constitute legal, clinical, or specialist behaviour support advice. It should not be relied upon as such.
All information is provided in good faith, however, we make no representation or warranty of any kind, express or implied, regarding the accuracy, adequacy, validity, reliability, or completeness of any information. The information pertaining to Autism and support methods must be individually determined by each person’s GP and specialist therapists, and is a very complex evolving context and support needs and methods are subject to change.
This article is not a substitute for professional advice from a qualified NDIS Behaviour Support Practitioner. You should always consult with an appropriate professional to address your specific circumstances. Under no circumstance shall Ability Therapy Specialists Pty Ltd have any liability to you for any loss or damage incurred as a result of the use of this information. Reliance on any information provided in this post is solely at your own risk. This article, website, and your participation are governed under the Client Booklet - Privacy Policy: Disclaimer, Terms, Conditions as a necessary provision under Australian service quality standards.
Double Gifted - And Fabulous
Rare to reframe complex diagnosis as giftedness - but this is all about perception. What you see is what you get. So why not see past the mask?
Reframing Dual Diagnosis as Giftedness
Many people with a dual diagnosis have both a disability and a mental health condition. Sometimes, this can make life harder. But what if we looked at it differently? What if we saw the special gifts behind these challenges?
Understanding Dual Diagnosis
Dual diagnosis means having two different issues at the same time. For example, a person might have autism and anxiety. Or intellectual disability and depression. These combined difficulties can be tricky to manage.
However, focusing only on the difficulties can make us forget the person’s strengths and talents. Every person has unique abilities that can shine when we pay attention.
Looking beyond the surface - the key to understanding self and others
Seeing Abilities and Strengths
When we reframe dual diagnosis as giftedness, we start to notice special skills. For example, many people with autism are very good at noticing details others miss. They might have a great memory or be strong at puzzles and patterns.
People with certain mental health challenges may have deep creativity or show enormous courage. These talents can help them and others in many ways.
Why Reframe Matters
Changing how we think about dual diagnosis matters for the person and their support team. When we see giftedness, we can build on those strengths to help the person grow.
This approach helps families, teachers and therapists provide better support. Instead of focusing on what a person can’t do, they focus on what the person can do.
Practical Steps to Appreciate Abilities
Listen carefully to each person’s interests. What do they enjoy? What makes them happy?
Encourage skills they already have. Join them in activities that use these strengths.
Create plans that include their talents. This can boost their confidence and make learning fun.
Conclusion
Dual diagnosis is challenging, but it is also a chance to see the amazing abilities in someone. By appreciating these gifts, we help people reach their potential. Focusing on strengths rather than limitations changes lives for the better.
Everyone deserves to be seen for their abilities. This way, we all grow together.
Dr Jo, PhD, is a senior Psychotherapist and Behaviour Support Specialist registered with the National Disability Insurance Scheme. He works from Armidale NSW Australia and consults across the country. He works with Dr Dwayne Kennedy with consultant services available online today. Send us a line via the form on Home Page.
"My situation is high-risk. Why don't I have a behaviour support plan?" Understanding NDIS Safety Plans vs. Long-Term Plans
Deep dive into why BSPs can take a while to create, how to engage the process, and ways to address the challenges to find help and work with the help when you find them.
Preface
This post is a special edition ‘Deep Dive’ into one of the many profound questions that come up often in our work. It provides a more comprehensive analysis that draws information together in one place, for those interested in reading further. We cite the sources as well - so all of the information provided here is up to date at the time of writing. Don’t trust our word on this however - always research the sources. The NDIS in particular is well known for changing regularly! We urge you to do your own research and keep informed.
Estimated Reading Time: 9-10 minutes
Reading Tip: Click on the articles - they open up to nice layout to read more easily.
Audio Tip: Use your favourite app to ‘read aloud’ - we suggest Google Read & Write as it has a solid free version and works with Google Chrome.
Image of a Black Page with the word ‘Plan’
Introductions
In today’s world introductions are often overlooked in their importance. While often these come at the end of articles, we’ve decided for good reason to introduce you to the author up front.
Dr Jorandi (Jo) Kisiku Joseph Randolph Bowers is a PhD in Health Counselling Psychotherapy, a qualification they earned from winning a doctoral teaching and research scholarship at UNE from 1998 to 2002. Doc Jo has three doctoral degrees, as well as many qualifications and years of experience. They worked full time as a Behaviour Specialist since 2012, well before the NDIS rolled out in Australia. His practice focuses often on highly complex cases with dual and multiple diagnosis.
Jo works with and founded Ability Therapy Specialists with another senior behavioural specialist, Dr Dwayne Wannamarra Andrew Kennedy. Dr Dwayne is a PhD in Counselling with many degrees in education and community based services. He has worked in disabilities since youth, and in specialist behaviour support since around 2016 with full time work in this area since 2018.
As many like to know more about the author, Jo earned a Doctor of Divinity in Ceramic Arts & Spirituality, received an Honorary Doctor of Divinity in Spirituality, and holds a Master of Education in Counselling Psychotherapy, Diploma in Ericksonian Hypnotherapy and Counselling, Practitioner Certification in Neuro-Linguistic Psychotherapy, and a Bachelor of Arts in Spirituality & Philosophy.
Jo is a NDIS registered specialist behaviour support practitioner and counsellor, senior honorary member with the Australian Counselling Association, senior fellow of the Australasian Society of Lifestyle Medicine, and author of over 250 works including a dozen books. Having worked in specialist behaviour support in the years prior to NDIS roll out, Joseph Randolph was asked by managers to stay in regional New England in NSW and set up a community practice. This led Jo to take up the work of Director and Senior Clinical Specialist with Ability Therapy Specialists Pty Ltd, a registered NDIS provider in Australia. Their work includes telehealth therapy for people across the country – often helping where waiting lists are extreme and in Australia’s most rural, remote and bush settings.
Jo is an author of over 250 works, with a dozen books including ‘Clay Art Therapy and Spirituality,’ ‘The Practice of Counselling,’ ‘Mi’kmaq Puoinaq Two Spirit Medicine,’ ‘Sacred Teachings from the Mi’kmaq Medicine Lodge,’ and ‘Solitude Awakens: The Heart, Forest, Mountain Way.’
A Guide for Participants and Families
We know that waiting for a behaviour support plan can be stressful, especially when you're managing high-risk situations. You may have heard about a "30-Day Rule" and are left wondering, "Why is my plan taking so long?"
This is a common and completely valid question. Here’s the simple answer:
That 30-day timeline is a specific legal safeguard that only applies when a 'restrictive practice' (like using locked doors, gates, or physical restraints) is involved. It’s a human rights rule to make sure those practices are monitored.
But what if your situation is high-risk, but doesn't involve those things? Does that mean you just wait?
Absolutely not.
Your provider's first legal and ethical duty is to your immediate safety. This is covered by different NDIS rules (the Code of Conduct and Practice Standards). In any high-risk case, a good practitioner's first step isn't to write a comprehensive plan, but to create an interim safety plan.
This "safety plan" is a vital document. It gives your support team and family clear, immediate steps on how to de-escalate and manage unsafe situations right now.
This immediate safety plan allows the practitioner to do the most important job: a proper assessment (we call it a "Functional Behaviour Assessment" or FBA) to understand the why behind the behaviour. A final plan written without this assessment is just guesswork.
In short: A "safety plan" comes first (for immediate risk). The full "behaviour support plan" comes later (for long-term change).
This article explores the details of these different NDIS rules. It's helpful for understanding your rights and what you should expect from your provider. For providers and other professionals, the fully cited analysis is included below.
Image of a person sitting with a laptop and puppy looking to the camera
Deeper-Dive Summary for Humans
For NDIS providers and practitioners, the "30-day rule" for behaviour support plans (BSPs) is a common point of focus. However, this timeline is widely misunderstood. Our analysis confirms this 30-day deadline applies only to cases involving a regulated restrictive practice (RP). This is a human rights safeguard, triggering the need for a lodged "Interim BSP" (Part 3, Section 12 of the NDIS (Behaviour Support) Rules 2018).
But what about high-risk cases where no restrictive practices are present? The Behaviour Support Rules do not set a specific deadline for these scenarios. Instead, urgency is dictated by a different, and often more immediate, set of obligations:
Provider's Duty: The NDIS Practice Standards (Core Module, Section 4: Risk Management) require providers to have a system to "identify, analyse, prioritise and treat" risks. A high-risk history (even if stable) is a known risk requiring proactive management.
Practitioner's Duty: The NDIS Code of Conduct (Section 1(d)) mandates a Duty of Care, requiring practitioners to "provide supports and services in a safe and competent manner, with care and skill."
Reactive Duty: If a high-risk behaviour does cause harm, the NDIS (Incident Management and Reportable Incidents) Rules 2018 (Part 2, Section 6) apply, requiring a Reportable Incident notification within 24 hours.
In all cases, the Functional Behaviour Assessment (FBA) must be completed before the Behaviour Support Plan (BSP). For the 30-day Interim BSP, the law explicitly requires it to be based on a "preliminary functional behaviour assessment" (Section 12(3)(a) of the Behaviour Support Rules). For high-risk, non-RP cases, best practice (driven by the Code of Conduct) involves an "interim safety plan" to ensure immediate safety and guide data collection for the full FBA.
Key Points
The 30-day (1-month) timeline is for lodging an Interim BSP and is triggered only by the use of a Regulated Restrictive Practice (RP).
Source: NDIS (Behaviour Support) Rules 2018, Part 3, Section 12(1).
This Interim BSP must still be based on a preliminary FBA. The FBA always comes first.
Source: NDIS (Behaviour Support) Rules 2018, Part 3, Section 12(3)(a).
For cases with no RPs (even if high-risk), the 30-day rule for BSPs does not apply. The Behaviour Support Rules timelines are tied to the lodgement requirements for RPs.
The urgency for high-risk, non-RP cases is driven by:
The provider's Risk Management obligations.
Source: NDIS Practice Standards, Core Module, Section 4: Risk Management.
The practitioner's Duty of Care.
Source: NDIS Code of Conduct, Section 1(d).
If a high-risk behaviour results in a critical incident, the 24-hour Reportable Incident timeline is the primary legal driver for an immediate response.
Source: NDIS (Incident Management and Reportable Incidents) Rules 2018, Part 2, Section 6.
Clinically, a practitioner should still create an "interim safety plan" for any high-risk case to manage immediate safety. This is a clinical best-practice tool derived from the duty of care, not the legislated "Interim BSP" document.
Navigating the Grey: Reconciling NDIS Timelines, High Risk, and the Functional Behaviour Assessment (FBA) -First Principles
For NDIS Behaviour Support Practitioners and providers, navigating the legislative landscape is a complex task of reconciling clinical best practice with a rule-based framework. A central point of confusion is the timeline for intervention, particularly in high-risk cases.
The framework, especially the NDIS (Behaviour Support) Rules 2018, appears to tie all urgency to the use of regulated restrictive practices (RPs). This leaves a critical question: What are the legislative provisions for a participant who presents with high-risk behaviours but has no RPs in place?
This article analyses the interplay between the NDIS Rules, Practice Standards, and Code of Conduct to clarify the required order of operations, with direct citations for verification.
Section 1: The "Known" Rule (The 30-Day RP Clock)
The most commonly cited timeline is the one-month (30-day) rule. This is found in the NDIS (Behaviour Support) Rules 2018, Part 3, Section 12.
What it is: This rule mandates that a behaviour support plan (an Interim BSP) must be lodged with the NDIS Commission.
When it applies: It is triggered only when a regulated restrictive practice is first used with a participant.
Source (Section 12(1)): "If... a behaviour support plan that provides for the use of a regulated restrictive practice... has not been developed, the NDIS provider... must ensure that... an interim behaviour support plan... is developed... and... a copy is lodged with the NDIS Commission... within 1 month after the use of the regulated restrictive practice..."
What it requires: A common misunderstanding is that this 30-day rush means the BSP is written before the assessment. This is incorrect. The Rules explicitly state the Interim BSP must be:
Source (Section 12(3)(a)): "...based on a functional behaviour assessment, which may be a preliminary functional behaviour assessment..."
The legislation correctly anticipates that a comprehensive assessment is impossible in 30 days. It therefore makes provision for a "preliminary FBA." This triage-style assessment allows the practitioner to form an initial hypothesis of function, identify immediate risks, and create a plan that, first and foremost, ensures the RP is being used as safely as possible.
The 30-day clock, therefore, is a specific human-rights safeguard triggered exclusively by the use of RPs.
Section 2: The Apparent "Gap" (High-Risk, No RPs)
This brings us to the core dilemma. What provision covers a participant with a history of severe self-injury, physical aggression toward others, or dangerous absconding, but for whom no RPs are authorised or in use?
If a practitioner searches the Behaviour Support Rules 2018 for a timeline, they will not find one. This is because the legislative urgency for this scenario is not located within the Behaviour Support Rules. The timelines in Part 3 (Interim) and Part 4 (Comprehensive) are structurally linked to the lodgement and oversight of plans containing restrictive practices.
To assume no urgency is required is a critical error. The urgency is simply driven by different, and often more immediate, legal requirements.
Section 3: The True Provisions for High-Risk, Non-RP Cases
In the absence of the 30-day RP clock, a practitioner and provider must turn to three other core pillars of the NDIS framework.
1. The NDIS Practice Standards (Proactive Risk Management)
This is the provider's primary proactive obligation. Under the NDIS Practice Standards and Quality Indicators, Core Module, Section 4: Risk Management, providers must demonstrate:
"Each participant’s support plan includes a risk assessment that identifies risks to the participant... Risks are managed through a risk management system... The provider’s risk management system supports the provider to identify, analyse, prioritise and treat risks..."
A referral for a participant with a "history of high risk" (even if currently stable) is a clearly identified risk. The provider's own NDIS-audited system legally obligates them to "treat" this risk. In this context, "treatment" is the commissioning of a specialist behaviour support assessment (an FBA) to proactively mitigate that risk.
2. The NDIS (Incident Management and Reportable Incidents) Rules 2018 (Reactive Response)
This is the provider's primary reactive obligation. If the participant's high-risk behaviour results in a "Reportable Incident" (RI)—such as those defined in Section 5 (e.g., "the serious injury of a person with disability")—an immediate legal timeline is triggered.
Source (Section 6(1) & 6(2)): The provider must notify the NDIS Commission of the RI within 24 hours of becoming aware of the incident.
Following this notification, the Commission will require the provider to detail the "remedial action" taken. This action would, by necessity, include an urgent clinical response, such as commissioning an immediate FBA and safety plan. In this scenario, the 24-hour RI rule provides a far more rapid trigger for intervention than the 30-day BSP rule.
3. The NDIS Code of Conduct (Practitioner's Duty of Care)
This is the provision that governs the individual practitioner. All NDIS workers and practitioners are bound by the NDIS Code of Conduct, which is a legislative instrument under the NDIS Act 2013.
Source (Section 1(d)): The Code requires that practitioners must:
"provide supports and services in a safe and competent manner, with care and skill."
A "competent" practitioner, upon receiving a referral detailing high-risk behaviours, has an ethical and professional duty of care. They must use their clinical judgment to triage this case at a high priority. De-prioritising the case simply because it lacks an RP—and therefore a legislative lodgement deadline—would be a failure to act with "care and skill."
Section 4: The Interim Plan Dilemma (Legislative vs. Clinical)
Given these provisions, why does the legislation not offer an "Interim BSP" provision for high-risk, non-RP cases?
The answer lies in the critical distinction between a legislative document and a clinical tool.
The Legislative "Interim BSP": This is a formal, legal document. Its sole purpose is to be lodged with the NDIS Commission to provide oversight for a human rights-impacting restrictive practice (as defined in Section 12 of the Behaviour Support Rules). Because there are no RPs in our scenario, the Commission does not require a document for lodgement. Therefore, the legislative provision is not "triggered."
The Clinical "Interim Safety Plan": This is a best-practice tool. It is what any competent practitioner should develop in any high-risk case. It is not called an "Interim BSP" and it is not lodged with the Commission.
This clinical document is mandated by the practitioner's Duty of Care (under the NDIS Code of Conduct). Its purpose is to:
Provide immediate risk-mitigation guidance to the support team.
Outline clear de-escalation strategies.
Establish the specific data collection methods required to complete the full FBA.
This interim safety plan is the provision. It is the first step in the FBA process, not a replacement for it.
Image of a lady on mobile phone at a laptop outside at table in garden
Conclusion: The Functional Behaviour Assessment (FBA) is Always First
The logical and legal progression for any behaviour support case is clear, though it requires looking at the entire NDIS framework, not just one set of rules.
The FBA is the Priority: A BSP—whether interim or comprehensive—can never be written without an FBA. The assessment always comes first. This is explicitly stated for Interim BSPs in Section 12(3)(a) of the Behaviour Support Rules.
The Trigger Defines the Timeline:
If RPs are present: The 30-day lodgement clock for an Interim BSP starts (Behaviour Support Rules, S12). The first job is a preliminary FBA.
If RPs are absent (but risk is high): The provider's Risk Management standards (Practice Standards, Core Module, S4) and the practitioner's Duty of Care (Code of Conduct, S1(d)) create the urgency. The first job is to create an interim safety plan based on a preliminary FBA.
If an incident occurs: The 24-hour RI rule forces an immediate organisational response (Incident Management Rules, S6).
Disclaimer
The content provided in this article is for general informational purposes only and does not constitute legal, clinical, or specialist behaviour support advice. It should not be relied upon as such.
All information is provided in good faith, however, we make no representation or warranty of any kind, express or implied, regarding the accuracy, adequacy, validity, reliability, or completeness of any information. The NDIS legislative framework, including the NDIS Act 2013 and associated Rules and Practice Standards, is complex and subject to change.
This article is not a substitute for professional advice from a qualified NDIS Behaviour Support Practitioner. You should always consult with an appropriate professional to address your specific circumstances. Under no circumstance shall Ability Therapy Specialists Pty Ltd have any liability to you for any loss or damage incurred as a result of the use of this information. Reliance on any information provided in this post is solely at your own risk. This article, website, and your participation are governed under the Client Booklet - Privacy Policy: Disclaimer, Terms, Conditions as a necessary provision under Australian service quality standards.
Thank You from Dr Jo - And Safe Holidays Ahead
We wanted to take this moment as we head to end of November - can you believe it? To say Thank You to all the people who supported our service this year with referrals and to clients who rely on our roles in their lives - a huge thank you.
Positive Behaviour Support 101
Positive Behaviour Support is awesome actually, and life changing for anyone who wants to have a go.
Seeing Strengths in Support
When we think about behaviour support, it often sticks to psychology as just a discipline. But there’s a better way to look at it.
A Person-Centred Approach
Person Centred Psychotherapy focuses on the whole person. It uses a strength-based approach. This means the language is friendlier, easier to understand, and more caring.
Enjoy each moment.
What Does Support Really Mean?
Support is about helping someone. It means enabling them and walking alongside them on their journey. Support is also about listening carefully. When we listen well, we open up new possibilities.
Working Together to Find Strengths
We create plans with the people we support. Even those with profound disabilities have strengths and abilities. Instead of looking at what’s missing, we look at what’s there. People often see the glass as half-empty. But therapy helps us see it as half-full.
Celebrating What You Can Do
Focusing on your skills feels good! You can celebrate what you already have. Then we ask, how can we build on that? Positive behaviour support moves from just managing problems to encouraging growth and change.
Being Different is Okay
What seems radical or different for one person might be normal for another. Only the person and their supporters truly know what works best. Skilled therapists can help challenge and support everyone.
Every person is different, same with flowers.
Transforming Disability into Strength
Don’t underestimate ability.
Turn what some see as a disability into strength and capacity.
‘Invig-ability’ means giving energy and life to someone who might feel stuck. It’s about moving forward with new energy.
That’s the path to real change.
Dr Jo is a Counselling Psychotherapist and registered provider with the National Disability Insurance Scheme.
Behaviour Support, for real.
Behaviour support for real life is balance and flow. Join Jo Bowers PhD to reflect on the mystery of finding the flow.
A Family Affair
One couple set their marriage at stake on the answer. One wanted to use a passive nurturing method. The other wanted to use firm discipline. And don't assume one is male and the other female. You would be wrong if you did.
Needless to say. The marriage ended at a stale mate. You know why?
Because nothing can last on extremes. If you want a marriage to work you need compromise. If you want behaviour support to work you need balance.
Balance of Factors
Not between extremes. To find balance you need reason and feeling in sync. Kids are not an abstract formula. Kids are real people with complex needs.
Too much of one. Things do not work. Too much of the other. Things do not work.
More Like a Circle
But not so much this and that - behaviour support is more about plus this and then more. You look for the whole view - the ways things flow in real life.
We call this ecology, some say ‘holistic.’
We think this perspective comes from observing life and relationships. And not a tad of wisdom. Buckets might help.
Nurturing the Flow
Structure and nurturing. Yes.
Boundaries and a bit of limited choices. Yes.
Freedom appropriate for the child's development. Yes.
But freedom is the partner of responsibility. Without one the other will fail.
So, it goes. The mix is unique for each child. Each person. Yet don't we want to get it right? Yes. Indeed.
Behavioural support in real life is about balance and flow. It is keeping relationships healthy, and finding ways to support our needs and the needs of others.
We look at the behavioural life of two-legged (humans) as highly flexible and yet given to patterns, routines, and cumulative processes. One things leads to the next, and the narrative is not always easy to understand.
About ATS
ATS is a registered behavioural specialist service under NDIS, with practitioners PhDs Jo Bowers and Dwayne Kennedy. We are members of the Australian Counselling Association, and the Australasian Society for Lifestyle Medicine. We work via telehealth with NDIS participants in behaviour support, counselling, and therapy assessment funded areas.
Life is a balance, sometimes even a dance.
How to Learn from Experience
Learning is fun! Who says? Here are ways to enjoy learning and change.
Here are a few simple steps to learning from experience - any experience at all.
Reflect on these questions while day dreaming, writing, drawing, painting, or creating something, even cooking.
What happened? Describe it.
How did you feel? What was your inner reaction?
What thoughts went through your mind during, and not long after?
How do you feel now about the experience?
What questions or unresolved issues remain, if any?
Some clients use this format for writing an email to a therapist. It gives them a more clear focus.
They end up learning heaps from the exercise, and then they get helpful feedback from their counsellor.
Learning is fun. Who says?
People who live with disability often learn through these steps.
Have an experience.
Repeat it.
Briefly talk about it, see if you like it.
Try it again. Repeat.
If it feels good, keep doing it.
The trick is not to think too much. Disability often involves making things simple, or things are kind of simple already.
When you think too much, it can complicate things. Just do it. Try it. Repeat.
Once behaviour becomes a habit - it sticks. You do not need to think too much.
Habits form fast when they are fun. It is when we are trying too hard to change that change gets hard.
But even shifting into a new habit to replace something not safe or helpful can be easier.
The key is to find the smallest way to change that is fun, feels better, and has a bit of motivation.
Motivation is everything.
Behaviour Support and Human Rights
Human rights are central to positive behaviour support. Here we review key values.
Behaviour Support does not exist in a vacuum.
All behaviour support happens in familial, social, community, legal, legislative national, and international policy contexts.
Simple but potent sign on a street post says it all - every human has rights.
Key Human Rights
Here are a few of the basic human rights involved in behaviour support practice.
These touch on relationships in families, communities, and nations. These come directly out of international, national, and state based policy and practice standards.
Every person has the right to:
Dignity and respect
Live in and be part of a community
Realise their individual potential and capacity for physical, social, emotional, intellectual, psychological, and spiritual development
Access services on an equal footing to others in society that support a reasonable quality of life
Choose their own lifestyle and to have access to information
Participate in decisions that affect their lives and future
Receive services in a way that results in least restriction of personal rights and opportunities and human freedoms
Address any grievance or complaint without fear or recrimination from service providers including fear of the discontinuation of services
Protection from neglect, abuse, exploitation, and harrassment
Citation: Behaviour Support: Policy and Practice Manual Part 1, NSW Department of Ageing, Disability and Home Care, 2009
Dr Dwayne and Dr Jo are PhDs and senior counselling psychotherapists and behaviour specialists, registered with NDIS so funding is available for NDIS participants. We work across Australia via telehealth - online using zoom, facetime or your favourite app. Get in touch via the form on home page.
Beautiful display of colour showing respect.
Beyond Talk Therapy - Getting Positive Outcomes
Therapy helps us in relationships and life, in practical ways. How vital this is during these times of change.
I Have Tried Psychology and Counselling for Years. I Have Talked Through My Problems Endlessly, and Nothing Has Changed.
Many people feel stuck after years of talking therapies. They may say, "I have tried psychology and counselling for years. I have talked through my problems endlessly, and nothing has changed." If this sounds familiar, you are not alone. While talking is important, practical change is what makes a difference.
Personal time is key. Relaxing with yourself.
Moving Beyond Talking
Talking about problems is helpful to some extent. It helps you understand your feelings and challenges. However, without action, nothing shifts. Our approach at Ability Therapy Specialists is different. We focus on practical behavioural change. We help you learn new skills that work in real life.
Practical Behavioural Change
We do not just explore your feelings. We work with you to find solutions you can try immediately. This could be changing a routine, building skills to manage stress, or learning new ways to communicate. We focus on what will work best for your everyday life.
Solutions That Fit Your Life
Every person is unique. What works for one may not work for another. That is why we tailor our plans to suit you. We involve you in making the plan. This way, you feel confident to use the strategies. Our goal is to make changes simple and achievable.
Having Fun While Changing
Change can be hard. It can feel overwhelming and tiring. We believe change should also be enjoyable. Our therapists bring creativity and fun into the process. Using games, activities, and positive reinforcement, we help you stay motivated. Learning new skills becomes a positive experience, not a struggle.
People love talking about their life - and good therapists actually listen!
Leaning Into Positive Change
Small steps can lead to big changes. We encourage you to lean into positive change at your own pace. Our support helps you celebrate every success, no matter how small. With consistent practice, new habits form, and life starts to feel better.
In Summary
If you have tried talking therapies without seeing change, consider a fresh approach. Ability Therapy Specialists offer practical, solution-focused therapy. We help you create real changes in your life. Together, we make therapy useful, fun, and effective. This approach empowers you to move forward, build skills, and enjoy a better quality of life.
Send us a line via form on home page.
Understanding Relationship Behaviour Support
Relational behaviour support is funded under NDIS as a practical solution focused service. Learn more here.
Relationship behaviour support is an important part of helping people with disabilities and mental health needs build positive connections with others. At Ability Therapy Specialists, we focus on providing practical strategies that improve interactions and reduce challenges in relationships.
What is Relationship Behaviour Support?
Relationship behaviour support involves understanding behaviours that affect how people relate to family, friends, carers, and others around them. It looks at reasons behind behaviours and works to promote respectful and positive communication.
All relationships need support - behaviour therapy is a practical way to help
Why is it Important?
Good relationships contribute to a person’s overall wellbeing. Difficult behaviours can lead to misunderstandings, frustration, and isolation. Support helps people express their needs clearly and develop skills to interact comfortably with others.
Who Can Benefit?
People with disabilities, mental health needs, parents, families, and support staff all benefit from relationship behaviour support. It helps everyone involved understand each other better and work together to solve challenges.
How Does It Work?
Our approach begins with listening to the person’s story. We then assess behaviours in everyday life to identify what causes stress or conflict. Using functional assessments, we create personalised behaviour support plans tailored to each individual’s needs.
Practical Solutions for Everyday Life
Support includes teaching practical skills such as:
Managing emotions
Communicating needs effectively
Building social skills
Responding calmly in difficult situations
We also provide guidance for families and carers on how to create supportive environments that encourage positive behaviours.
Using Telehealth and Online Services
Ability Therapy Specialists offer telehealth and online consultations to reach people nationwide. This means support is accessible regardless of location, enabling consistent help for clients and their support networks.
We meet you where you are at - on your device. One day soon, in your eye glasses too.
The Role of Behaviour Support Plans
A behaviour support plan is a detailed guide that outlines strategies to encourage positive behaviour and reduce challenging behaviour. Plans are regularly reviewed and updated with input from the person and their team.
Working Together for Success
Relationship behaviour support is most effective when everyone involved collaborates. This includes the person receiving support, family members, carers, and professionals. Together, we create a respectful and understanding environment that nurtures positive connections.
Contact Ability Therapy Specialists
If you or someone you care about needs help with relationship behaviours, Ability Therapy Specialists offer expert guidance and practical solutions. Our professional team supports you to improve everyday interactions and build stronger relationships across Australia.
See our contact form on the home page and get in touch. We are NDIS Registered for funding using your NDIS Plan.
Understanding Behaviour Support
Behaviour support is really practical and life-changing because the approach builds on skills and abilities.
Behaviour support is a way to help people whose actions or behaviours are causing problems in their lives.
Sometimes, behaviours become too intense, happen too often, or last for a long time.
When this happens, it can affect a person’s quality of life and even their physical safety.
Behaviour support focuses on understanding these behaviours and finding ways to improve the situation.
Our clients meet us online - sharing intense and real life events. This is life-changing work.
When Is Behaviour Support Needed?
People may need behaviour support if their behaviours:
Happen very often (high frequency)
Last for a long time (long duration)
Are very strong or intense (high intensity)
These behaviours might cause harm to themselves or others. They can also make it hard for the person to take part in everyday activities, enjoy life, or be safe.
How Behaviour Support Helps
Behaviour support uses different strategies to help the person and those around them. The goal is to reduce the intensity, frequency, or duration of difficult behaviours. This can make life safer and better for the individual.
Support often begins by understanding why the behaviour happens. People don’t act in difficult ways without a reason. Behaviour support specialists look at what might be causing the behaviour, such as:
Health issues
Communication difficulties
Environment or setting
Emotional needs
What Behaviour Support Includes
Behaviour support can include:
Functional assessments to understand behaviour triggers and needs
Creating behaviour support plans that are safe and practical
Teaching new skills or ways to communicate
Training families, staff, and others who support the person
Regular reviews to see how well the plan is working
Practical therapy is more than good intentions - it is making real life changes that matter.
Benefits of Behaviour Support
Effective behaviour support can:
Improve safety for the person and others
Enhance the person’s independence and participation in daily life
Reduce stress and anxiety for the person and their support network
Offer practical solutions to everyday concerns
Conclusion
Behaviour support is about helping people whose behaviours affect their safety and quality of life.
By understanding the reasons behind these behaviours and working with the person, families, and support staff, behaviour support can create positive changes that make life better and safer.
At Ability Therapy Specialists, we are committed to providing professional, respectful, and practical behaviour support to help individuals reach their full potential.
Get in touch with Dr Dwayne and Dr Jo via the form on home page, or give us a ring and leave a message.
What is Functional Assessment of Behaviour - Why Do I need it?
Functional assessment of behaviour is really helpful. Here is why.
Most Practical and Useful of All
Base your effort on a functional assessment - and your intervention is twice as likely to be useful.
Said another way, get a functional assessment of behaviour and your path to change can be easier. Not always true in every case of course, but the general wisdom holds. The more we get what is happening - the easier it is to make changes.
Struggling with a behavioural problem is no fun, and can be dangerous to health and safety. The path to change and learning can sometimes be hard. Therapy is here to make this process a bit more manageable.
Solid Assessments are Key
By useful we mean that behaviour support based on solid assessment and intervention planning seeks to
1. increase safety wherever possible,
2. provide insight and hope,
3. create options and choices, and
4. reduce behaviours of concern and/or change environments and supports that then contribute to changes in behaviours.
In many cases these positive outcomes are documented by the behavioural therapist. This is accepting the fact that every situation is unique and that there are no guarantees.
Vital Assistance - Key Insights
Research and professional practice - over many years - shows that counselling and behaviour support assessments and interventions provide significant assistance to clients, families, and staff.
Smith et al (2016) looked at the relationship between biological setting events and problem behaviours.
Then they worked through a "functional analysis of each participant’s problem behaviour in relation to two context factors: fatigue and task demands."
By implementing a multi-component intervention to address both the biological setting factor and the behaviours of concern they reported a dramatic reduction in problem behaviour. The implications show that understanding and assisting with setting events contributes to addressing behaviours of concern.
No doubt life is complex at times - we simplify things so the path is a bit easier.
What You Know, What You Need to Know
In behaviour support, what you know is often not enough. People in everyday life miss the boat. That is natural. We are not trained to see what is underlying in behavioural patterns.
Specialists are trained and with experience to pick up on the patterns, to investigate the data, to uncover the motivations. These insights help sort what is happening. More important - how to make changes more easily.
Source: Christopher E. Smith, Edward G. Carr, Lauren J. Moskowitz, 2016, Fatigue as a biological setting event for severe problem behavior in autism spectrum disorder, Research in Autism Spectrum Disorders, Volume 23, March 2016, Pages 131–144.
Dr Jo and Dr Dwayne are senior counsellor psychotherapists and behaviour specialists - focused on real life therapy with people in everyday life via your smart phone or devices. They work on zoom, facetime or your fav apps. They reach out across Australia and are paid via your NDIS Funding Package Plan. Their private books are closed at the moment but let them know if you are interested in therapy - maybe they can find room to assist. Contact via the form on home page.
Great thing about assessment is - the therapist does the hard work.
Behaviour Support and Counselling Telehealth in Perth and Western Australia
We are so happy to open services for NDIS participants in Perth up to Broome and across WA - here is how you can engage.
Living in Perth or anywhere in Western Australia offers many benefits, but access to specialised therapy and behaviour support services can sometimes be challenging due to the vast distances involved.
At Ability Therapy Specialists, we bridge that gap through our professional telehealth services.
Tailored Hours for Western Australia Clients
Our telehealth sessions are structured with your convenience in mind. For clients based in Perth and throughout Western Australia, we typically schedule appointments during business hours from 8 am to 2 pm local Perth time. This timing ensures that you can easily fit therapy sessions into your day without disrupting essential routines, school, or work commitments.
If you happen to coordinate with others in the eastern states, please note that our workday hours adjust to 10 am to 4 pm Sydney time. This flexibility means our support can function seamlessly across time zones without compromising quality care.
We are delighted to work with NDIS participants in Perth and across WA - providing specialist behaviour support and counselling
Access Senior PhD Specialist Assistance Nationwide
Unlike many local-only providers, Ability Therapy Specialists offers the exceptional advantage of accessing senior clinicians with PhD-level expertise and decades of hard won experience. No matter where you are in Australia - you can enjoy this advantage.
With telehealth, distance is no barrier to receiving high-quality, evidence-based assessments and therapy.
Our team specialises in service delivery to people with disabilities and mental health needs, as well as their families and support networks.
Whether you are in a remote region of Western Australia or in metropolitan Perth, you gain access to practical, tailored solutions informed by years of clinical research and direct experience.
Why Choose Our Telehealth Services in WA?
National Reach: No matter how remote your location in WA, our services come to you in your home.
Convenient Scheduling: Dedicated appointment windows aligned with WA business hours.
Expert Support: Receive guidance from highly qualified clinicians, including those holding PhDs.
Comprehensive Services: Therapy, behaviour support plans, functional assessments, and ongoing consultations.
From Perth to Broome, we honour the spirit of Australia and are delighted to connect in service as senior specialist counsellor psychotherapists
Serving the Vast, Beautiful State of Western Australia
Western Australia’s vastness and natural beauty are unique, but accessing specialist therapy doesn’t have to be difficult.
We encourage families, support staff, and individuals across this great state to embrace telehealth as a reliable, effective way to achieve meaningful outcomes.
If you seek expert assistance from senior specialists who understand your specific needs and circumstances, contact Ability Therapy Specialists.
Our telehealth service is your pathway to professional support that transcends distance and time zones.
Ability Therapy Specialists is an NDIS-registered provider committed to offering equitable, accessible therapy and behaviour support services for all Australians who make this connection with our tailored boutique service.
Experience the advantages of telehealth — expert care is just a call or click away. Use our Contact form on Home Page, we look forward to hearing from you.
Supporting Families Across Brisbane and Queensland in Behaviour Support and Counselling
Brisbane and Queensland NDIS participants benefit by accessing our specialist senior therapy support - here is how you can too.
At Ability Therapy Specialists, we proudly support families across Brisbane and throughout Queensland, specialising in telehealth online therapy for complex and specialist cases. Being based in northern NSW is no barrier - we work with people across the country.
We recognise the unique challenges that mothers and fathers face when raising children with special needs.
That’s why we provide tailored parenting coaching designed to empower and guide parents every step of the way.
Tailored Parenting Coaching
Parenting a child with special needs can be overwhelming.
Our specialised coaching focuses on equipping mothers with practical strategies and emotional support.
We explore personalised approaches that work best for each family, helping to build confidence and resilience in daily parenting.
We love helping NDIS participants and their parents in Brisbane and across Queensland with counselling and specialist behavioural therapy - get in touch today
Compassionate Counselling and Behaviour Support
Our experienced team offers compassionate counselling and behaviour support to individuals with autism and other disabilities.
We develop customised behaviour support plans that address specific challenges, aiming to improve daily functioning and enhance quality of life.
Our focus is on solutions that are effective and easy to implement within everyday routines.
Accessible Telehealth and Online Services
Understanding that families may be spread across different locations, we provide accessible telehealth and online services.
This ensures that expert support from our team is available wherever you live in Queensland.
Our remote therapy sessions and consultations offer convenience without compromising the quality of care.
Practical and Personalised Solutions
At Ability Therapy Specialists, we believe every family deserves personalised therapy and comprehensive behaviour support.
Our approach is holistic and practical, designed to meet your family’s individual needs.
Whether it’s through one-on-one coaching, assessment, or ongoing therapy, we work collaboratively with you to achieve the best possible outcomes.
Every family needs a community of support to raise their children
Ability Therapy Specialists
Choosing the right support team is crucial for your child’s development and your family’s wellbeing.
Ability Therapy Specialists is known for expert guidance, compassionate care, and tailored interventions.
Together, we can help navigate the complexities of disability and mental health needs with solutions that truly make a difference.
Find our contact form on the home page or give us a ring.
Servicing Melbourne and Victoria for Behaviour Support and Counselling
ATS works with clients in Melbourne and Victoria, meeting real needs via telehealth provisions. Here is how you can get involved.
Specialist Behaviour Support at the Ready
At Ability Therapy Specialists, we proudly support NDIS participants across Melbourne and Victoria with tailored telehealth and online services designed to meet your unique needs.
Whether you or your family require therapy, behaviour support plans, or functional assessments, our experienced team delivers practical, evidence-based solutions directly to you, no matter where you are.
ATS works with clients in Melbourne and Victoria to assist with personalised therapy
Diverse Challenges - Personalised Support
We understand the diverse challenges faced by people with disability and mental health conditions, and we work closely with participants, families, support workers, and staff to provide personalised care that promotes independence and wellbeing.
Our NDIS registered services include:
Telehealth counselling and therapy sessions
Comprehensive behaviour support planning
Functional assessments and goal-oriented strategies
Support for families and carers to navigate daily challenges
Serving Victoria and Melbourne community members, we are committed to accessible, efficient, and compassionate support that fits your lifestyle.
Connect with Ability Therapy Specialists to ensure your NDIS plan is maximising your potential with expert guidance every step of the way.
Supporting Greater Sydney NDIS Participants
ATS works with clients in greater Sydney and is delighted to assist - here is key information on how to apply.
Access Expert NDIS Telehealth Behaviour Support and Counselling Services
NDIS participants in Greater Sydney can now access specialised therapy, behaviour support, and counselling services without the lengthy wait times commonly experienced in metropolitan areas.
Based in Northern NSW, Ability Therapy Specialists offers convenient telehealth and online appointments, delivering high-quality support directly to your home or preferred location.
We are delighted to assist NDIS participants in greater Sydney NSW
Key Benefits for Sydney-Based Participants:
Bypass Long Waiting Lists: Skip delays often faced with in-person services in Sydney by accessing immediate telehealth appointments.
Flexible Scheduling: Choose times that fit your lifestyle, reducing travel time and disruption.
Comprehensive Support: Receive therapy, behaviour support plans, and functional assessments tailored to individual needs.
NDIS Registered: Fully compliant services that meet the requirements of your NDIS plan.
National Access: Benefit from expert care delivered seamlessly across state lines from Northern NSW to Sydney.
Experience timely, professional, and personalised support without the wait.
Connect with Ability Therapy Specialists to maximise your NDIS plan and improve outcomes through convenient telehealth services.
Choosing an NDIS Behaviour Support Provider: A Guide for Participants & Families
Educational insights to help your choose providers based on quality factors in counselling and behaviour support services.
Choosing the right NDIS behaviour support provider is important for achieving meaningful outcomes. Services can differ in delivery, expertise, and approach. The industry culture is informed by quality reviews and standards.
This guide outlines key quality factors to consider when comparing providers. For the sake of learning we provide an easy comparison between two providers.
Provider 1 example demonstrates strengths. Provider 2 shows what is often available and could be improved.
Service Delivery
Personalisation
Provider 1: Tailored truly person-centred support plans developed by PhD-level clinicians with decades of real-life experience.
Provider 2: Standardised plans with less individualisation.
Service Scale
Provider 1: Limited caseloads with focus on relationship building with world-class quality to ensure focused attention.
Provider 2: Larger caseloads may reduce individual focus.
Delivery Mode
Provider 1: Primarily telehealth, no travel for clients, in-home access on your device, offering flexibility nationwide.
Provider 2: Combination of in-person and telehealth; may be location-limited.
Personalised therapy where you need it - in your home and daily life.
Expertise and Qualifications
Clinical Expertise
Provider 1: PhD-level clinicians with extensive experience with relevant specialisations.
Provider 2: Varies; may include psychologists, OTs, or social workers.
Specialisations
Provider 1: Person-centred experts with diverse specialisations and focus on complex cases and dual diagnoses.
Provider 2: Generalist approach across conditions.
Industry Recognition
Provider 1: Highly regarded for expert reports, clinical assessments, behaviour support plans, funding and plan reviews.
Provider 2: Recognition varies; may not specialise in complex cases.
Therapeutic Approaches
Therapy Modalities
Provider 1: Integral-cognitive-holistic, solution-focused outcomes, with creative methods (art, clay, gaming, symbols).
Provider 2: Primarily traditional talk therapy.
Innovative Techniques
Provider 1: Uses innovative methods to enhance engagement, learning, and personalised outcomes.
Provider 2: Standardised interventions.
Engagement Strategies
Provider 1: Focus on enjoyment, learning, empowerment, motivation, and positive life-changing outcomes.
Provider 2: Typically behaviour modification focused.
Personalised access to counselling and behavioural therapy now is critically important.
Accessibility and Support
Service Availability
Provider 1: Flexible scheduling often employed to meet client needs, with texting, video, and email access.
Provider 2: Fixed hours; flexibility may be limited.
Family Involvement
Provider 1: Active therapy-process engagement and guidance for parents, siblings, and families.
Provider 2: Family involvement varies; may be optional.
Geographic Reach
Provider 1: Services available nationwide via telehealth - while our Sydney timezone focus this a bit - this is adaptable.
Provider 2: Limited to specific regions.
Wherever you are - we are there with you. Therapy is not just person-centred, it meets real needs and nurtures change.
Conclusion
When you compare all the above quality indicators, you would probably choose Provider 1. Maybe Provider 2 sounds familiar in some or many ways. The point is to evaluate what you need and to seek a provider if you can who demonstrates more strengths.
Selecting an NDIS behaviour support provider or a counsellor for that matter involves considering service delivery, expertise, therapy approaches, and accessibility. There are many quality indicators that typify the industry - not just from the counselling and behaviour therapy sides.
These quality frameworks include the NDIS Commission Quality Standards Framework. Ask your provider how they square with the NDIS Quality Framework review and how they did on their last NDIS external audit.
Call to Action
To explore how ATS can support your family, please contact us or learn more about our services.